When people hear that I am a travel health nurse, they often imagine me travelling to every country in the world administering vaccinations, while lounging on a beach, catching a tan. However, my work is much more dynamic and varied than that and I am certainly not lounging on a beach administering vaccinations to people.
But wouldn’t that be the dream?
Behind every travel consultation, I find I have to use my intuition, problem-solve various travel health issues and keep up to date with the latest travel health information. This allows me to educate my clients so they can make a holistic decision on their health before, while and after they travel.
In this article, I want to give you an insight into my typical day as a travel health nurse and what it can look like for me. I would like to remind you that every travel health professional’s journey is different and what I may experience in clinic doesn’t necessarily mean every health professional goes through the same thing. Please remember that I work in a private travel clinic setting and this can also be different for those working in NHS/primary care environments. Our individual journey is unique to each and every one of us and I am here to give you a look at just a small piece of the day in the life as a travel health nurse. So, hop into my backpack and let’s head on a little adventure.
So, what does a typical day look like for me?

My day usually starts before my clients arrive at the clinic. First, I need water. I cannot function without water as I get so dehydrated throughout the day. This can be common when I am talking constantly and have back-to-back consultations, which can cause me to have a dry mouth.
Once my water bottle is filled, I will carry out my everyday clinic checks such as fridge temperatures, anaphylaxis kits, cleaning rota and make sure I am fully stocked with all the important items I need to keep myself organised throughout my shift.
It is important that I stay organised and that I have all the equipment, vaccinations and medicines at hand. If I am unorganised, it means my consultations can become discombobulated. As I live with dyslexia, being disorganised can quickly throw me off track, so I always start by looking through my diary and reviewing my client appointments for the day.
This will involve:
For me, I need to ensure I have the recommended travel health pages open on my computer so it is easier for me to stay focused and keep structure during my consultation. It will also enable me to concentrate and provide the necessary information to the clients without getting distracted.
Every itinerary tells a different story. A consultation with a honeymoon couple travelling to Tanzania will look very different from a client who is travelling for a business trip to Bangkok or a student taking a gap year around South America.
Before my consultations, I will check the NaTHNaC (Travel Health Pro) website, the World Health Organisation (WHO) and any email updates for changes, which may impact my client’s travel itinerary. For example, if there is a malaria outbreak or a vaccination shortage, it is important for me to be aware of this so I can properly advise my clients. Keeping up with changes in the clinic’s Patient Group Directions (PGDs) and following the Green Book is essential in making sure I adhere to policy and that I am administering the correct vaccinations to the appropriate person(s).

My consultations are back-to-back this morning. Yikes! It’s a good job I have water.
My first travel health consultation is advising a couple on how to prepare for their safari in Kruger National Park in South Africa. Luckily, they have received their recommended NHS vaccines and only want to know about malaria tablets. But have they weighed up their risk of rabies? They are taking part in a controlled safari guided tour and will be using transport to get around and staying in a 5-star hotel and I have discussed with them what to do if they get bitten or scratched by a warm-blooded animal. What do you think their risk of contracting rabies will be?
But wait! The clients throw me a curve ball. They divulge to me that they are currently trying for a baby and think it will be romantic to conceive while they are away.
I have 1 hour (which isn’t too bad) to organise myself, gather all the information I need from the clients and relay all the important travel health information to them. Asking questions about their current medical status is vital in making sure I can give them the best information they need.
Questions I ask and explore include:
You can always refer to the Malaria prevention guidelines for travellers from the UK by the UK Malaria Expert Advisory Group (UKMEAG) for more information.
As a travel health professional, what other questions would you ask?
It’s always handy to think about the big picture so you can gain a clear understanding of the client’s medical status and what information you can give them. And I love to find out how other travel health professional approaches their consults and what questions they may ask so I can implement it into my own consultations.
However, sometimes there are questions you may forget to ask after the client has left the building…
BUT DON’T PANIC! You can always follow up with the client by giving them a call or emailing them the important information such as (in this client’s case), travelling while pregnant, the associated risks and pre-travel preparation etc. You can find such information in the links below:
Luckily, they don’t need a yellow fever vaccine as there is no risk of the disease in South Africa.
BUT WAIT! Are they transiting through a high-risk yellow fever county, which has been listed on the WHO website as a yellow fever certificate requirement? The client confirms that their flight will be transiting via Dubai, which poses no risk of yellow fever therefore a yellow fever certificate will not be needed. Phew, I don’t need to talk about the yellow fever vaccine.
Asking the all-important questions is vital for me to also assess what I don’t need to talk about as it will allow me to discuss other potential travel health issues and help me organise my time efficiently.

During the next consultation, I advise a student who will be completing their final medical elective placement in a hospital in Bangkok, Thailand.
It’s always lovely when a client is travelling to one of my favourite destinations and Thailand is very special to me as this is where my husband and I celebrated our honeymoon together. I ask the client a lot of questions such as:
Luckily my client is organised and has already received their hepatitis A, typhoid and Td/IPV (tetanus, diphtheria and polio) vaccines with their GP practice and has finished their course of hepatitis B with their occupational health advisor at their university hospital placement. My client is mainly here to start their rabies course and after assessing their risk, discussing with them the doses, cost, administration of vaccine, potential side effects and pre and post exposure rabies treatment, they were happy to start the first dose. I inform them about other practical travel advice such as how to avoid insect bites, maintain good food and water hygiene, how to manage jet lag and what to pack in their medical kit.

My next client is a delivery driver travelling to Senegal to visit their wife. They have been separated from each other since covid and finally this is their window of opportunity to meet again after all this time.
A real challenge for me is my accent as I have a strong Liverpudlian dialect and sometimes people may struggle to understand what I am saying. Especially if a client only speaks a little English or may not be familiar with my accent. This can sometimes be tiring for me as I have to make sure I speak slowly, repeat sentences and write notes down so I am confident my client understands all the information I am providing to them.
As my client speaks limited English, it is imperative that they have an interpreter with them during their consultation, especially when a discussion needs to be had around dengue, yellow fever, zika and malaria transmission. Senegal is high risk for all these diseases and it is important for me to discuss with them:
Having a sensitive discussion around these topics is vital due to the potential complications my client and their partner may face if they were to experience a pregnancy. It’s important to approach this conversation with respect for local cultural and religious views, while acknowledging that local guidance may differ. Education is key and as you can see, there are many layers of travel health information to take into consideration to ensure the client is safe and is given all the information they need to make a holistic decision.
How would you approach your client about sexual health in this scenario?
Would you feel comfortable talking about methods of sexual protection? Or is this an area you feel you may need to build more confidence in and improve your communication skills? Again, we are all learning and I am always interested to see where I can improve or to look at how confident I have become in certain areas and skillsets of travel health medicine.
I have written a blog titled ‘STI Prevention – How comfortable are you talking about Sexually Transmitted Infections during your consultations?’, to help travel health professionals better approach the topic of sexual health discussions.

Yay, I have time to catch up with my notes and process blood results from the current university students we have been conducting occupational health assessments with alongside a rabies clinic, which will last until lunch at 13:30. These appointments are only 10 minutes each as:

As you have read so far, not all consultations are simple. Many of my travellers have complex health backgrounds that can make things more complicated, but they also keep my day interesting.
I have conducted travel health consultations with a range of clients who:
These cases often take more time. Sometimes I consult with our on-call medical team to weigh up the risks and benefits. And occasionally, I have to suggest changing travel plans if the health risks are simply too high. These types of consultations are never easy but my priority is always my client’s safety.

I have a walk-in client who has lost their yellow fever vaccination certificate and requests a new certificate re-issued as they are travelling tomorrow to Tanzania. Tanzania can sometimes present a complex situation with Yellow Fever requirements, as it not always straightforward depending on their travel route. I will refer to this client as Mr X to save any confusion. I hand their predicament over to my colleague as I have a client already waiting, who is travelling to Peru and will be climbing Machu Picchu.
One of my main concerns for people climbing Machu Picchu is altitude sickness, as people are climbing over 2,500m above sea level and their potential risk of altitude sickness is greater the higher they climb. Although Machu Picchu is around 2,430m, many visitors ascend quickly by flying straight into Cusco (~3,400m) or trekking via the Inca Trail (~4,200m), increasing their risk. Now, I have found from previous appointments, that people who plan to climb Machu Picchu don’t really take the risks of altitude sickness seriously. They believe it is an issue for places like Mount Kilimanjaro so I need to make sure I inform them on the associated risks.
My client has decided to obtain Diamox (Acetazolomide). I explain that, while it’s licensed in the UK for other conditions, using it to prevent acute mountain sickness is off-label.
Under our clinical protocol, we are able to supply this medication following a full risk assessment, and I provide them with an information sheet that details this off-label use so they can give informed consent. They are still happy to obtain the medication today as they want to be prepared. I love an organised traveller and it’s nice to see when they make a choice about their own care

Luckily this appointment lasts 20 minutes as the client is all up to date with their previous vaccinations and they confirm to me that it was their purpose of buying Diamox during today’s visit. To my alarm, Mr X is still in the waiting room and to my surprise they are unable to provide any documented evidence of their past yellow fever vaccination and my colleague has searched our database to find that we don’t have any history of yellow fever vaccination being administered.
Mr X explains he is travelling to Tanzania, with an overnight stop in Kenya. While Tanzania doesn’t usually require a yellow fever certificate for travellers arriving directly from the UK, those entering from countries where yellow fever is present, such as Kenya, must show a valid certificate on entry.
Turns out Mr X only had a consultation with us a few years prior but did not the obtain the vaccine. They realise they received it at another clinic as the vaccine cost less than at our clinic.
But as what mostly happens when a client is stressed and unorganised, they often blame the nursing staff. It is now my job to be professional but firm and highlight the next stages to Mr X and how they can gain proof of a yellow fever vaccine certificate. They can either:
As a full yellow fever assessment needs to be completed in an adequate time frame, what I don’t want to do is rush my assessment with them.
It is important for me to explain the associated risks and conduct a thorough assessment without pressure or stress on my part.
However, I cannot see them at this moment in time as my next client, who is travelling to Morocco and would like the rabies vaccine, has arrived for their appointment and my other colleagues are now with their own clients so they are unable to see Mr X. I explain to them that I have available appointments at 16:30 but to my surprise Mr X sighs and says ‘forget it’ and walks out of the building, slamming the door.
I assume Mr X has decided to try their luck at the other clinic or decided against re-vaccination. Dealing with demanding clients who have not retained their documents or followed through on advice can be part of the job, and maintaining professionalism is key.
I’m starting to get lethargic. My brain usually gets tired around this time in the afternoon, especially if I have back-to-back appointments. It is important for me to have mini breaks throughout the shift as I live with dyslexia and my brain can get tired easily from talking all day and looking at computer screens. Our clinic is situated in a basement with limited access to windows so nipping outside for daylight is essential. So, I grab my cup of water and head outside.
I see a few returning university students for their occupational health vaccines, which is nice and simple as they only require their hepatitis B vaccine. It gives me time to catch up with the rest of the blood results and with any emails.
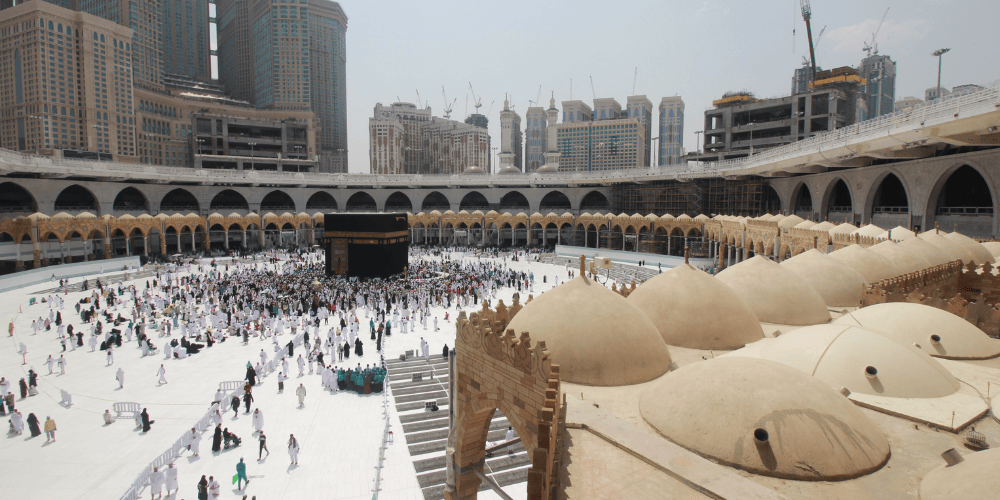
I see on my calendar that a client has booked in for the 16:30 time slot however it is not Mr X. My next appointment is with a child, who needs a Meningitis ACWY vaccine for their visit to Saudi Arabia for Hajj with their parents. Now if you’re anything like me, when it comes to vaccinating children, it has never been my favourite aspect of travel health nursing and I am happy to admit that I have never felt completely comfortable doing it.
I find my anxiety builds, while waiting for the child to attend clinic, as I don’t know what to expect. Will the child be calm and collected or will they scream and shout the building down? But all that anxiety passes when the child arrives with mum and they turn out to be the most angelic individuals.
Mum is a calm person and immediately places boundaries with their child (I love this). When it comes to administering the vaccine, mum is able to hold the child in a stable position, while I administer the vaccine in a quick and safe fashion. Phew! I’m happy that worked out.
How do you feel about vaccinating children?
I use to feel embarrassed about addressing this concern as I was afraid that my colleagues would think badly of me but I soon found out there were a lot of other travel health professionals that are in the same boat so please don’t worry if you feel the same way, you are not on your own.
But you can find ways to help your confidence when it comes to conducting consultations with children in clinic:
I have included some handy links below for blogs, which have been written by our travel health experts Alys Bunce; Ten tips for dealing with appointments that involve injecting children and Michelle Hunter; How to administer vaccinations to infants and children safely?.
Some travel health professionals even feel nervous discussing children’s immunisation schedules with parents, however the more experience and shared learning we gain, the more confident we become in these conversations.
With their newly completed Meningococcal ACWY certificate and vaccinated arm, both child and mum leave happy and I can finally start the end of day shutdown of the clinic, check fridge temperatures and make sure the clinic is re-stocked. The hover and mop is out and within 20 minutes, the clinic is looking brand spanking new again.
With the tills cashed up and the alarms set, it’s time to head home.
For me, being a travel health nurse is about more than administering vaccinations and dispensing medications. It’s about my client’s story, their journey and the connections I make with them. Every consultation for me is an opportunity to empower someone to travel safely and confidently.
Travel health nursing is never the same. By the end of the day, I often spend time reading any travel health updates, attending training sessions or catching up with the latest guidelines. A region that was safe from malaria yesterday might report an outbreak tomorrow and I enjoy keeping up to date with it all as I love to travel myself.
Behind every safari, mountain trek or work trip abroad, there is often a travel health professional (like me and you) working behind the scenes, making sure that our client’s adventure doesn’t turn into a life-or-death situation. And to be honest, for me, this is what makes travel health medicine so rewarding.
Giving you written and video content to answer all your questions on primary care education from Phlebotomy to Travel Health.
Subscribe now to be kept updated with our latest posts and insights.
Notifications