
If you take blood or give injections it’s very likely that at some point you will have performed (or are going to perform) these sharps-based procedures on someone who is living with HIV. And you will likely have a set of perceptions about that. Be prepared to see (and avoid) some discriminatory practice.
The short answer should be NO: As long as you are treating everyone (including yourself) as if they have a blood borne infectious disease when handling sharps, then you would do everything exactly the same.
There are two notable points here though:
So, Let’s start with what HIV is and why people worry about blood contact when performing injections or phlebotomy. Then we will look at infection control precautions around sharps use.
HIV (human immunodeficiency virus) is a virus that damages immune system cells and weakens the ability to fight infections and disease. AIDS (acquired immune deficiency syndrome) is the term used to describe a number of potentially life-threatening infections and illnesses that happen when the immune system has been severely damaged by the HIV virus.
AIDS cannot be transmitted between people. But the HIV virus can.
HIV is found in the body fluids. This includes semen, vaginal and anal fluids, blood and breast milk. However, it is an unstable virus and does not survive outside the body for long. HIV cannot be transmitted through sweat, urine or saliva. The most common way of getting HIV in the UK is through having anal or vaginal sex without a condom.
Treatment has improved drastically since the onset of the epidemic in the 1980’s which saw many deaths and illness from HIV and consequent AIDS. The memory of this tragic time lingers on, and a lot of people still have an image in their minds that is not congruent with the reality of what HIV is today.
Most people these days who are living with HIV will lead long and healthy lives if they are on effective treatment, which has come on in leaps and bounds over the years. It’s easier to control than living with Diabetes, usually just one pill a day keeps it at bay.

The goal of HIV treatment is to have an undetectable viral load. Undetectable equals untransmittable (U=U). This means that the level of HIV virus in the blood is too low to be detected in a test. For people living with HIV, if they have been taking effective HIV treatment and the viral load has been undetectable for 6 months or more, they CANNOT pass on the virus. So, even a needlestick injury where a health care worker or patient has come into blood-to-blood contact with HIV via a sharp will result in a zero to very low risk of transmission.
And, just to note, even if they WERE to contract HIV, it’s not the most worrying of diseases to have these days. There are much much harder-to-manage ones they should be worrying about. More about this later.
Well, it can be pretty dire. There are countries that have entry requirements and will deny entry or residence if a person has a positive HIV status. Check out this website to look at some of those places. Some countries will confiscate HIV medications on arrival. Some will put you in prison. These countries perpetuate stigma and discrimination against people living with HIV by highlighting HIV to be a “dangerous disease”. Treatment opportunities can be lower in other places. Therefore, HIV in some countries is still under-treated with more visible consequences. And the vicious cycle continues.

We might assume that HIV discrimination only goes on abroad, but it’s happening right here in the UK too, in a subtle but equally pernicious manner. In a clinical setting too, where medical professionals should really know better.
As a phlebotomy and immunisation teacher, I find that there is not a session that goes by (especially a phlebotomy one) where someone doesn’t mention a discriminatory practice that they have seen or performed in the workplace relating to people living with HIV. Here are some of the things I have heard in the last year.
(Please note, these are NOT acceptable or necessary measures in clinical practice):
“We use new sharps bins every time for HIV patients. As soon as the procedure is done, we seal them up and dispose of them”
“In our surgery, we ask HIV patients to bring their own sharps bins and take them away again”
“We double-glove for the HIV patients”
“We ONLY wear gloves for the HIV patients”
“I refuse to take blood from HIV patients. Only the more experienced staff do that”
“I use smaller needles to reduce the risk”
“I usually put the sharp back in the tray and then take it to the sharps bin after. However, with HIV I take the sharps bin with me and dispose of the needle straight away.”
“We always warn staff before they are about to take blood from someone with HIV. We flag it on the records and booking notes”
“We don’t have our HCA doing bloods or injections. She has HIV and might pass it on to the patients”
Imagine how this feels for a person living with well-managed HIV whom has no symptoms, feels well and has undetectable (therefore untransmittable) levels of HIV. To have someone say, “can you provide your own infectious sharps waste receptacles and let me put on an extra pair of gloves…” . Especially if a person with a far more infectious disease is sitting next to them in the waiting room, yet is welcomed in with open gloveless arms…
What about if you’re a staff member excluded from performing procedures and enhancing your skill set for no reason other than the outdated stigma behind your diagnosis? An equally awful outcome of this is the perpetuation of low self-esteem and internalised stigma that a person might have of themselves.
If any of the above quotes have shocked and disappointed you then that’s ironically a good thing. You know your stuff!
If any of the quotes unfortunately sound familiar then it’s perhaps time to review some clinical practice that could not only be discriminatory, but against the law.

The final push to write this blog came just after World AIDS day (1st December 2022) from reading an opinion piece in the BMJ. It stated that in a survey, only “16% of the public knew that someone with HIV on effective treatment can’t pass the virus on”. The author points out that “Education and knowledge about living with HIV today has not kept pace with developments”

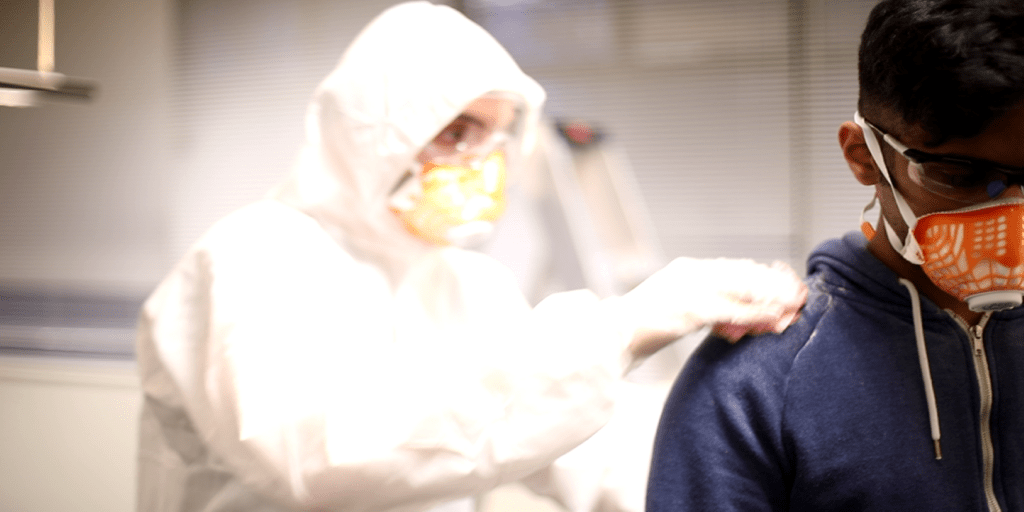
Consider this: Hepatitis B is around 100 times more infective than HIV. Hepatitis B virus is much hardier than HIV and can hang around on surfaces for up to 7 days (unlike HIV which dies very quickly after being exposed to the air). Malaria is spread through the blood. Marburg, Ebola, Hepatitis C, Syphilis; these too are blood borne diseases. Furthermore, people do not always know they are carrying a disease and may be asymptomatic (enter: COVID-19 and mask-wearing, for example, or google “typhoid Mary” and why hand washing around food preparation areas is important). So, because of this we use standardised Universal Precautions and should do so with every patient. This way, there is no discriminatry practice and everyone remains as safe as possible.
There is consensus among the national guidance on infection control that certain universal precautions are a must. For example, NICE sets out a lengthy and comprehensive set of guidance encompassing both immunisaiton and phlebotomy procedures. For example, the use of Aseptic Non Touch Technique (ANTT) for clinical procedures.
For immunisations the national guidance indicates:

All the standard injection precautions for immunisation are in the Green Book.
Nothing should be any different when practicing as someone with HIV, or performing a procedure involving sharps on a person living with HIV.

For phlebotomy, the procedure involves accessing the circulating blood supply (a vein) directly -and for a longer period. Therefore, exposure risks are considerably higher and a higher quantity of blood is likely to be met with. The site of the puncture can bleed more vigorously and in larger amounts. The needles have large hollow bores which when retracted are filled with blood (unlike an immunisation which will be filled with medicine).
So, for phlebotomy it’s slightly different:
Find more details in the comprehensive WHO guidance on Phlebotomy.
Again, you should do NOTHING differently where HIV is concerned.
Regardless of medical status, both procedures require having an understanding of universal precautions to take around sharps-use.
Both procedures involve having a sharps bin nearby, where the singly-used puncture device can be disposed of into immediately.
And both procedures require that sharps bins are not overfilled, and are sealed properly when full.
Hand hygiene is a must between all patients.
And ultimately, both procedures require that a person (or equally a staff member) with HIV is treated with dignity and respect and that NO discriminatory practices are used.
So, is it time to review your practice or give a colleague a nudge? Discriminatory practice is happening every day in relation to HIV and sharps use. Be on the look out and let’s nip this in the bud.
Remember U=U.

https://www.brigstowe.org/hiv-awareness-training/
https://www.nat.org.uk/our-work/training-and-learning
https://www.tht.org.uk/our-work/training
https://ght.org.uk/positively-speaking-hiv-awareness-training
Giving you written and video content to answer all your questions on primary care education from Phlebotomy to Travel Health.
Subscribe now to be kept updated with our latest posts and insights.