Measles is an extremely contagious viral disease than can lead to serious complications and in some cases death. It is especially dangerous in infants and children under five, pregnant women and those who are immunocompromised. Measles, once on the brink of eradication, has made a troubling comeback in recent years. Despite the availability of a reliable and affordable vaccination, over the last decade we have seen surges of measles cases and fatalities, with outbreaks occurring worldwide. This resurgence poses a significant threat to public health, both in the UK and globally.
What is measles?

Measles is a viral illness which is spread by airborne or droplet transmission mostly through coughing and sneezing. Measles is highly contagious, in those who are non immune, up to 90% of people would also become infected with the virus following close contact with an infected individual.
What are the symptoms and complications of measles?
Initial symptoms can include a fever, runny nose, cough, red-watery eyes and a characteristic rash. Whilst the disease can be mild in many (though usually unpleasant), it can lead to serious complications in certain higher risk groups. Potential complications of measles can include otitis media, pneumonia, meningitis and encephalitis. Even though it is rare, encephalitis can cause additional issues including seizures, hearing loss, vision loss, and brain damage. Pregnancy complications can include a higher chance of miscarriage, stillbirth, or premature delivery. Measles can also lead to a very rare but potentially fatal disease of the central nervous system which can occur many years after developing the infection known as Subacute Sclerosing Pan-Encephalitis (SSPE).
Not only this but measles virus can also damage and suppress the immune system leaving individuals more vulnerable to exposure to other infectious diseases. It is thought that the damage measles causes to the immune system and the long term complications of this can last for as long as 3 years.
It is estimated that around 1 in 15 will have complications from the disease and up to 1 in 5 children will be hospitalised. In high income regions of the world such as Western Europe, measles causes death in about 1 in 5000 cases but as many as 1 in 100 will die in the poorest regions of the world.
Measles outbreaks worldwide
Since 2016, cases of measles globally have been on an upwards trend. 2019, in particular saw the largest reported measles cases recorded since 1996 (869,700 cases including an estimated 207,500 deaths, a 50% rise from 2016).
During the COVID-19 pandemic cases of measles largely declined. However with health-care efforts shifted to the control and treatment of COVID-19, routine immunisation programmes were impacted. The World Health Organization (WHO) reports that in 2021, nearly 61 million measles vaccine doses were postponed or missed due to COVID-19-related delays in immunisation campaigns across 18 countries.
2022 saw large outbreaks spread across Europe, with measles cases linked to music festivals and the restart of large public events and social gatherings. In 2023, large outbreaks have continued to be reported globally. In the last year we have seen a 30-fold rise of measles cases in the WHO European region in 2023 in comparison with 2022. Continuing transmission of measles in African countries and large outbreaks across India and other countries have also been documented.
Measles outbreaks in the UK

Within the UK, there has been a concerning increase in measles cases over the last year, with a large proportion of cases in the London area and in more recent months an outbreak has grown in the Birmingham area.
There is concern a significant outbreak could occur, particular amongst teenagers, young people and under vaccinated communities. Susceptibility is especially high among people aged 19 to 25, who were affected by false allegations about the Measles, Mumps and Rubella (MMR) vaccine in the late 1990’s, and some may still be unvaccinated.
This spike is a stark reminder of the importance of maintaining high vaccination coverage to protect vulnerable populations, especially children and those with compromised immune systems.
Why is there a rise of cases?
Several factors contribute to the resurgence of measles, and understanding these can help us to guide effective prevention strategies:
VACCINE HESITANCY: Misinformation and concerns about vaccine safety have led to lower vaccination rates. Addressing these concerns through clear communication is important.
INCOMPLETE IMMUNISATION SCHEDULES: Some individuals may not have received the recommended two doses of the MMR vaccine, leaving them susceptible to infection. Ensuring individuals are offered vaccination and opportunities to catch up is vital.
INTERNATIONAL TRAVEL: Measles can easily cross borders with travellers. Encouraging vaccination before international travel is essential.
COMMUNITY TRANSMISSION: Measles spreads rapidly in communities with low vaccination rates. Identifying and containing outbreaks swiftly is crucial.
Rates of vaccination worldwide
The current situation is critical, measles remains a significant threat to all countries, it is one of the most infectious human diseases known and can spread rapidly across populations and across borders, and it is almost entirely preventable through vaccines.
However due to failing immunisation rates and a decline in surveillance since COVID-19, there is now an “imminent threat” of measles spreading around the world and it remains an immediate concern globally.
No WHO region has achieved and sustained measles elimination. Since 2016, measles outbreaks and transmission have returned to 10 countries that had previously reported eradication of the disease.
In order to achieve and sustain measles eradication, coverage of 95% or higher of two measles containing vaccination is required. With just 83% of children receiving their first dose of the measles containing vaccine and only 74% receiving their second, globally the world is well under the proposed target.
Whilst coverage varies between countries, this is worryingly the lowest global coverage rates since 2008 and is a huge setback in worldwide efforts towards attaining and sustaining measles eradication.
Rates of vaccination in the UK
In the UK, we have seen a significant drop in vaccine uptake for MMR, vaccination rates, also impacted by the Covid-19 pandemic, are the lowest they have been in a decade.
The WHO set out a 95% vaccine coverage target. In England, coverage of two MMR doses at the age of five years is around 85%, with roughly 10% of children in the country unprotected from measles by the time they are ready to start school, with the rate in London being over 20%. According to 2022-23 figures, 89% of two-year-old children in England received their first dose of the MMR vaccine. There are some areas and groups where coverage of the 1st MMR dose at 2 years of age is as low as 69.5%.
How effective is the vaccine?
A single dose of measles-containing vaccine is at least 95% effective in preventing measles cases, a second dose will provide immunity to those who did not respond to the first. Over the last twenty years vaccination has dramatically reduced the number of deaths from measles. Since 1990 (when measles killed 872,000 people worldwide), it is estimated that over 1 in 5 of all child deaths averted worldwide have been due to measles vaccination, with the WHO estimating that between 2000 and 2021, 56 million deaths were avoided.
What more can we do as healthcare professionals to help to minimise measles outbreaks?

As healthcare professionals, in particularly as those working in primary care, we are at forefront of preventing, diagnosing, and managing measles cases and we can play a crucial role in curbing the spread of this highly contagious virus. Some of the key actions we can take include:
Enhance Surveillance for Measles Outbreaks
We must stay vigilant for signs and symptoms of measles. In the UK, measles is a Notifiable Disease. Any suspected cases of measles must be reported to your local Health Protection Team for rapid response. Anyone with a suspected or confirmed measles case should be encouraged to stay home and isolate, in particular avoiding contact with pregnant and immunocompromised individuals. Further information can be found in the UK Health Security Agency (UKHSA) National Measles Guidelines.
Educate the Community and Collaborate
It is important that we work to provide accurate and accessible information about measles, its symptoms, and the benefits of vaccination. We can do this through various communication channels to reach a broad audience, participating in vaccination campaigns and community outreach initiatives and working closely with local health departments to monitor and manage outbreaks.
Promoting Measles Vaccination
It’s important to counter vaccine misinformation by providing accessible scientific evidence. We need to take every opportunity to help individuals to make well-informed and balanced decisions about vaccines. We can emphasise the importance of the MMR vaccine to all eligible individuals and/or their parents/caregivers. By initiating conversations with these hesitant groups and addressing any concerns with evidence-based information we can help to dispel myths.
Reviewing Vaccination History and offering Catch up Vaccines
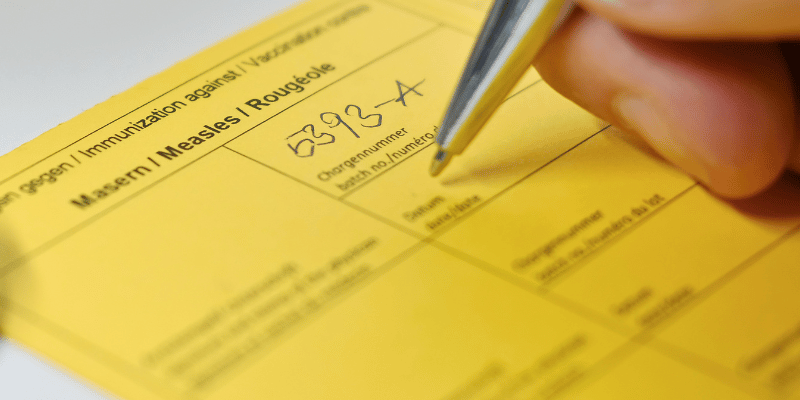
We can help to identify individuals who may be under-immunised or due for booster and schedule catch-up vaccinations to ensure complete protection. In some areas of the UK where outbreaks have occurred or with known low-immunisation rates, targeted catch up programmes have been running to try to boost population immunity.
Those working either within primary care settings or travel health clinics, are key to identifying at risk individuals. Travel is a great opportunity to ensure that individuals are up to date. People are coming to us to ask our advice, find out about prevalent diseases and their risks and how they can protect themselves – it’s crucial that measles is not neglected in this discussion.
Remember: you are never to old to vaccinate against measles. In the travel clinic where I work, a large majority of people when asked if they have had the MMR vaccine will answer yes, even though many were born in a time when it was not routinely given. A lot of people just assume they have had it.
So who would have had the MMR vaccine?
Don’t forget the MMR vaccine didn’t routinely become available in the UK until 1988, even then it wasn’t until the mid 1990’s that 2 doses were considered to be a complete course. Many young people born in the 1990’s or early 2000’s were also subject to the controversies and misinformation about any potential link with autism – all of which has now been disproved – however the lasting effects of this mean many are susceptible to these diseases.
Those born between 1980-1990 therefore may also not be protected against mumps or may have only had one dose of MMR. Whilst those born between 1970-1979 may have been vaccinated against measles (and for some rubella), or may have been exposed to mumps and rubella in childhood, offering natural immunity, many may still be susceptible.
Individuals born prior to 1970, would likely not have routinely had vaccinations (unless offered as a catch up when older) however likely may have had the diseases themselves when younger. However, with no proof or certainty, it is often much safer to assume that they are vulnerable to infection and to vaccinate (assuming no contraindications to receiving a live vaccine). Particularly if travelling to high risk areas or partaking in activities that put them at increased risk, such as staying with friends or family or mixing with the local population.
Travelling Infants

Whilst the first dose of MMR vaccine is not routinely given until 12 months of age in the UK. Infants who are travelling to countries where measles is endemic or to an area where there is a current outbreak can be considered for an MMR dose earlier if indicated (from 6 months of age). If this is the case, then the dose at 12 months and 3 years and 4 months is still recommended.
Likewise children who have received their first dose but not yet their booster can also have this brought forward. However if they are under 18 months and the booster is given within 3 months of their first dose then the pre-school vaccination is still advised. Further information can be found in the Measles Guidance on the Gov.uk website and the Travel Health Pro NaTHNaC Measles information page. The Green Book chapter on Measles also provides a comprehensive summary of how to adapt from the UK childhood schedule in more risky circumstances.
Many of the recent cases in the UK have links to travel so it’s important to address this risk in travelling infants and catch up any individuals who do not have history of either vaccinations or the disease.
In summary

Measles remains a global threat, in particular if vaccination rates were to fall even further. There is also an increased risk in travellers visiting countries with high rates of circulating disease and the disease then being brought back into the UK. The resurgence of measles demands a collective effort from healthcare professionals, the government and the community at large. As healthcare professionals who provide care, we are trusted individuals, therefore we need to speak up about the benefits and importance of vaccination. By staying informed, promoting vaccination, and actively participating in outbreak response efforts, we can play a pivotal role in mitigating the impact of this preventable disease.
Further Information on measles outbreaks
If you want to stay up to date further information on measles risk when travelling can be found on the outbreaks section for each country on both the TRAVAX and Travel Health Pro (NaTHNaC) websites. For a summary of recent measles cases and population incidence more information can be found through the following websites; WHO: Provisional monthly measles and rubella data and European Centres for Disease Control and Prevention- Monthly measles and rubella report. Data from UK cases can be found on the Gov.uk website.
Interested to learn more?
Why not sign up to one of our courses! At Health Academy we offer specialist courses on all the latest in Immunisation and Travel Health, from Virtual and Face-to-Face through the E-learning. Click on the images below to find out more.
Immunisation Courses
Travel Health Courses
Why not reflect on your learning from this article as part of your continuing professional development (CPD). Click below to fill out a short form which can be emailed to yourself for your own records.
CPD Reflective Practice