
Assessing pain in children is a complex and often misunderstood area, and it’s something we don’t always get right. Paediatric pain is frequently mismanaged, largely because children may struggle to pinpoint where their pain is or express it in ways that differ from adults. A distressed or upset child can leave us questioning whether they’re in pain, scared, or reacting to something else entirely.
Pain assessment in children is multifaceted and requires careful consideration of their age, developmental stage, possible cause of pain, and the behaviour of parents or carers. Children can pick up on parental anxiety, which may heighten their distress—being mindful of this and working to ease it can make a significant difference.
This is especially relevant in primary care settings, where nurses are often the first point of contact for children experiencing pain, whether from illness, injury, or routine procedures like immunisations. Recognising pain early and implementing effective interventions can make a significant difference in reducing distress and improving outcomes.

Assessing pain in children differs massively depending on their age and developmental stage. Utilising the correct pain assessment tool is vital, as using the wrong one for the wrong age can underestimate a child’s pain, leading to undertreatment. Naturally, the longer a child remains in pain, the more distressed both they and their parents may become, ultimately making pain management more difficult.
The three main pain assessment tools used for children are:
The choice of assessment tool depends on the child’s age and development, with different literature offering varying guidance on which tool to use for pain assessment. Regarding FLACC, some sources suggest it is intended for children aged 0–2 years, while others recommend its use postoperatively for children aged 2 months to 7 years, as well as for non-verbal children. Additionally, Great Ormond Street Hospital (GOSH) has revised the FLACC tool to better assess pain in non-verbal older children.
The Wong-Baker FACES® Pain Rating Scale is generally validated for use in children aged 3 and older. However, in practice, it is often used for children as young as 2, as they may still be able to understand and engage with the scale when guided appropriately. This practical adjustment allows for a more flexible approach to pain assessment in young children who may not yet have fully developed verbal communication skills.
The Numerical Scoring System should be used for older children who have the cognitive ability to understand and accurately respond to questions about their pain level. This method requires the child to comprehend the concept of rating their pain on a scale from 1 to 10, making it most appropriate for those who can engage in abstract thinking and make meaningful distinctions between different levels of discomfort.
It is important to recognise that, while literature provides guidance on pain assessment tools, each child should be assessed individually. These guidelines serve as a reference rather than a strict rule, as not every child will fit neatly into a predefined framework. In some cases, alternative assessment tools may be necessary to ensure an accurate evaluation of pain. As our understanding of pain assessment evolves, amendments and personalised approaches can be tailored to meet the needs of individual patients. Additionally, involving pain teams as well as specialists in paediatric pain assessment can be beneficial, particularly for children with complex conditions.
Below is an overview of how to use each of these pain tool assessments.

The FLACC pain assessment tool consists of five components: Face, Legs, Activity, Cry, and Consolability. Observing the child for one minute while using this tool helps determine their pain level.
FLACC has five components, each scored on a three-point scale, leading to a total score of 10. Below is a breakdown of each category:
When using this tool, you observe the child and assign a score (0–2) for each category:
Each category is scored from 0 to 2, leading to a total pain score from 0 to 10:
With this pain tool, context is key. Is the child crying and moving due to pain, fear, or both? Does the child settle when comforted by a parent? Involving parents in the assessment can be extremely valuable.
Great Ormond Street Hospital (GOSH) has developed a revised FLACC pain assessment tool designed for children and young people with cognitive impairments. This adaptation allows for a more tailored and child-specific approach to assessing pain in those who are unable to verbalise their discomfort, ensuring they receive a more accurate and appropriate evaluation.

When using Wong-Baker FACES®, it is important to try and build a rapport with the child for an accurate assessment. Being at the child’s level, using a soothing, friendly voice, and engaging in conversation can help establish trust.
The Wong-Baker FACES® scale consists of a series of faces with different expressions, ranging from a happy face (no pain) to a crying/distressed face (worst pain).
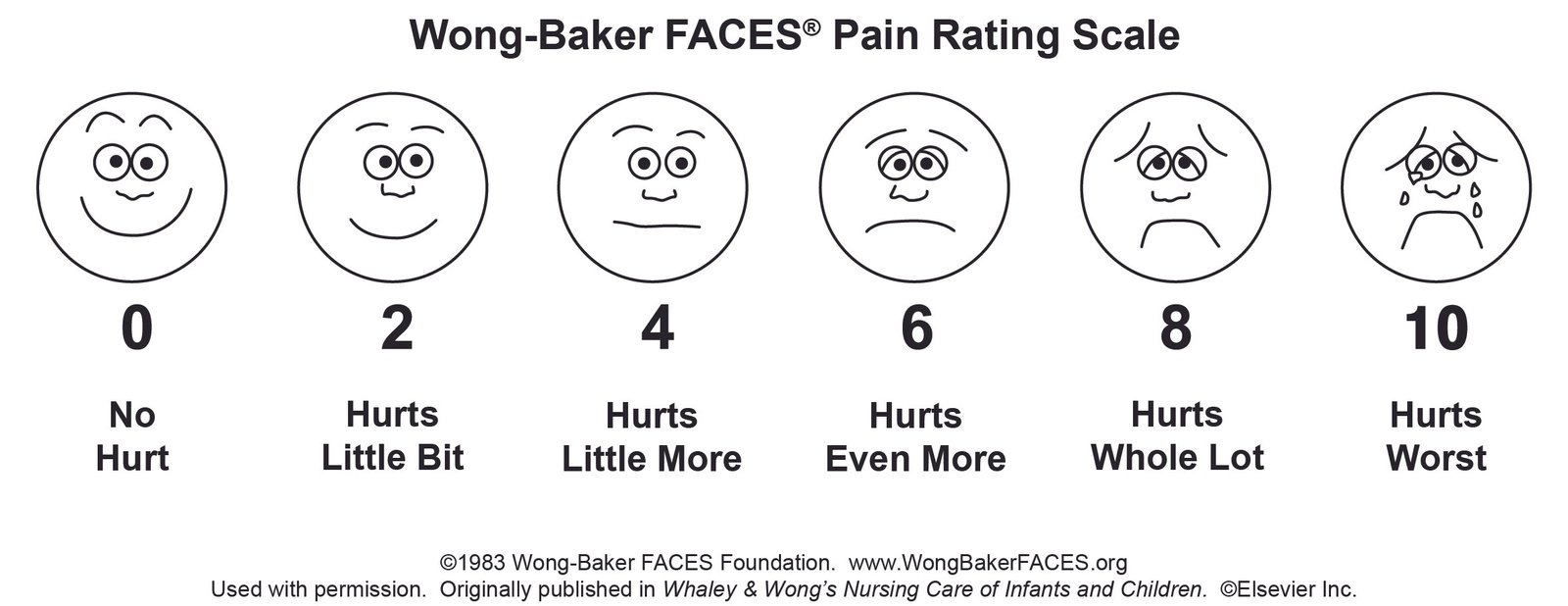
To use this tool:
Alongside using this tool, it’s helpful to ask open-ended questions like:
This helps avoid leading questions such as “Is this sore?”, which may cause the child to respond “yes” to everything. Additionally, it allows for a clearer understanding of exactly where the child is experiencing pain. However, it is important to be mindful that young children can sometimes become confused about the location of their pain and may point to any part of their body. Since this tool does not rely on verbal communication, children can simply point to the face that best represents their pain level. Encouraging parents to support their child during the process can also be beneficial in ensuring a more accurate assessment. Please note, however, that this tool is not intended to be used by a third party (e.g., parents, healthcare professionals, caregivers) to assess the patient’s pain. There are other tools designed for that purpose.

This system is used for older children who are able to understand numerical scoring. As children develop verbal skills, assessing pain becomes easier.
The Numerical Pain Scale is straightforward:
Explaining the severity of each number when asking the patient to choose helps ensure they give an accurate response, rather than just picking a number at random.
If the child struggles with numbers, then it is probably best to use the Wong-Baker Scale as this is easier for the child.
Using the correct pain assessment tool is essential to ensuring that pain is accurately recognised and effectively managed. Selecting the most appropriate tool based on the child’s age, developmental level, and communication abilities allows for a more precise evaluation of their pain experience. However, pain assessment should never rely solely on a scoring system; it is equally important to consider the broader context.
Observing the child’s behaviour, such as facial expressions, body language, and responsiveness, can provide valuable insights into their level of discomfort, especially for those who are non-verbal or have cognitive impairments. Additionally, parental input plays a crucial role, as caregivers often have a deeper understanding of their child’s typical behaviours and pain responses. Their observations can help validate the assessment findings and guide appropriate pain management strategies.
By taking a holistic approach that combines standardised assessment tools with clinical judgement and family involvement, healthcare professionals can ensure that pain is effectively identified and treated, ultimately improving the child’s overall comfort and well-being.

Once the severity of pain has been assessed and we understand how the child might be feeling, the next step is managing the pain and getting on top of it. Many people assume pain is only managed pharmacologically, but this isn’t the case.
Distraction, play therapy, topical analgesia, and parental involvement are just a few additional ways to help. In many cases, multiple forms of pain management may be required—for example, comfort positioning and distraction for immunisations, cold therapy and reassurance for minor sprains, or soothing techniques and analgesia for ear infections.
Another pain relief for young babies and neonates is the use of sucrose (sugar). Sucrose is commonly used to manage pain in young infants, especially during minor procedures like heel pricks or vaccinations. When given orally, sucrose activates sweet taste receptors, triggering a calming effect and reducing pain perception. This simple intervention offers immediate relief, making it especially helpful for infants who are unable to verbally express pain.
For older children cognitive-behavioural strategies (CBT) are effective for managing pain. Techniques like cognitive restructuring, relaxation, and distraction help reduce pain perception. Encouraging coping strategies through positive reinforcement and goal setting empowers children, enhancing their ability to manage pain and build resilience. These methods, alongside other pain relief approaches, offer a comprehensive solution for paediatric pain management.
Some of these non-pharmacological techniques may seem obvious, yet they are often overlooked, with clinicians jumping straight to pharmacological remedies.
Understanding how pain works is key to treating it effectively. When someone gets hurt, the body releases chemicals that send a pain signal through the nerves to the spinal cord (transduction). This signal then travels to the brain (transmission), where it is recognised as pain (perception). To help reduce it, the brain releases natural painkillers like endorphins and serotonin (modulation).
By targeting each part of the pain process and using multiple forms of pain relief together, we can manage pain in the best way possible.

At this stage, simple physical interventions can be an effective first response to pain. Methods such as applying a cold compress, immobilising an injury, or cooling a burn with water can provide immediate relief and help minimise discomfort. Since pharmacological options do not take effect instantly, these initial measures can play a crucial role in managing pain while further interventions are put in place.

Distraction is a powerful yet often underutilised tool in pain management, particularly in children. Their natural ability to focus on engaging activities can work to an advantage, reducing their awareness of pain. Effective distraction techniques vary by age, ranging from toys, games, and cartoons to guided imagery or deep breathing exercises for older children. Using age-appropriate strategies can significantly alter how pain is experienced and processed.
At this stage, pharmacological pain relief works by interrupting pain signals as they travel through the nervous system. The effectiveness of different interventions depends on the level of pain and individual response.

Pharmacological pain management is crucial for both mild and severe pain, often used alongside other strategies. For mild pain, medications like paracetamol or ibuprofen provide effective relief. For more moderate or severe pain, stronger pain relievers such as codeine, diclofenac, or morphine-based drugs may be required. These treatments should be closely monitored due to potential side effects. The choice of pain relief should be guided by local policies and tailored to the child’s specific condition. Factors such as the child’s age, medical history, and the nature of the pain influence the choice of medication. Adhering to local guidelines ensures safe and effective treatment while considering the individual needs of each child, ensuring personalised care that aligns with best practice standards.
A combination of pharmacological and non-pharmacological approaches is often beneficial, with pain relief methods complementing one another. Strategies such as distraction, comfort measures, and physical techniques can enhance the effectiveness of analgesia, creating a more comprehensive and personalised approach to pain management

Assessing and managing pain in children is challenging due to their varying age, development, and ability to express pain. Using the correct pain assessment tool is crucial to avoid underestimating pain and ensuring appropriate treatment.
Pain management involves a multimodal approach, combining pharmacological and non-pharmacological methods. First-line medications include paracetamol and ibuprofen, with opioids reserved for severe pain. Non-medication strategies such as distraction, play therapy, parental involvement, and topical anaesthetics are equally important.
Understanding the pain process—from transduction (injury) to perception (brain recognition) and modulation (pain relief response)—allows for targeted interventions. First aid addresses pain at its source, while distraction techniques reduce perception, and analgesia interrupts pain signals.
Using a combination of techniques is often the most effective way to manage pain in children, ensuring they feel as comfortable as possible while reducing both their pain and overall distress. By tailoring the approach to the child’s needs, we can provide better relief and create a more positive experience for them and their families.

Interested in joining us to learn more about Paediatric Assessment and Minor Illness? Contact us today to see how we can help you! Our expert-led specialist training is designed to boost your knowledge and confidence in assessing and managing paediatric patients effectively.
Click below to find out more about the Paediatric & Young People courses that we offer:
Our ‘Assessment of the Child in Primary Care’ course is designed to equip healthcare professionals with the knowledge and skills needed to navigate paediatric assessments confidently. Covering common conditions, signs and symptoms, participants will learn the fundamentals of conducting comprehensive assessments and managing various paediatric presentations in primary care settings.
Sold Out
Our ‘Paediatric Minor Illness’ course aims to provide nurses and healthcare professionals in general practice with essential skills for assessing and managing common paediatric minor illnesses. Participants will develop practical skills in history taking, assessments, and diagnosis to safely and effectively manage minor childhood illnesses in a general practice setting.
Sold Out
Our ‘Minor Illness in Young People’ course aims to provide nurses and healthcare professionals with essential skills for best practice in assessing and managing adolescent health complaints. Participants will gain practical expertise in history-taking and clinical assessments for safe and effective diagnosis of common minor illnesses in general practice.
Sold Out
Giving you written and video content to answer all your questions on primary care education from Phlebotomy to Travel Health.
Subscribe now to be kept updated with our latest posts and insights.
Start typing to search courses, articles, videos, and more.