If you have administered vaccinations previously you may be aware that there are some vaccines that are thought to be more painful than others. You may have even possibly heard one of the following phrases from one of your vaccine recipients:
“wow, I didn’t feel that one at all”
“ouch, that one really hurt”
“that one left me with a really dead arm for days”
So what is it that causes the pain from a vaccination? and why is it that some vaccines are possibly perceived as being more painful, and others may hardly hurt at all?
What causes a vaccine to be painful?

“Pain is whatever the experiencing person says it is, existing whenever and wherever the person says it does”
McCaffery, 1968
Pain it itself is a very subjective matter, everyone experiences pain in different ways and what causes pain for one person, may not for another. Measurements and expressions of pain in itself are also very hard to quantify which makes it a difficult subject to research.
It is thought that one of the contributing factors to whether someone finds a vaccine painful is actually down to the individual themselves. We have all probably given a vaccine to someone without them experiencing any pain and then given the same vaccine minutes later to someone else who found just the opposite, so why is this?
- Some people are extremely needle-phobic, and their fear of needles and injections can be quite distressing to them. It is commonly thought that fear and anxiety can actually heighten pain experienced, when anxiety levels are elevated, heart rate and blood pressure can rise which is thought to increase pain sensitivity.
- Moreover, those who are needle-phobic can often actually anticipate pain. There is some evidence to suggest that this can cause nerves to actually expect pain that is greater than what is really experienced.
- Additionally, when someone is fearful or anxious, they are more likely to tense up their muscle during vaccination. Injecting into a relaxed muscle rather than a contracted muscle is suggested to potentially decrease the level of pain felt.
Why some people feel more pain than others or experience a stronger inflammatory response can also be down to individual variants. It is known that age can decrease immune responses. However, research on the how’s and what’s of vaccine reactogenicity suggests BMI, genetics, gender and prior immunity to a disease can also have a possible contributing factor to the side effects experienced.
“It’s just a scratch” – why are some vaccines more painful than others?

Whilst the physical act of a needle breaking through the skin into the layers of fatty tissue and muscle can in itself be a possible source of pain. It is suggested that the variations in pain between vaccines may be down to the different physiochemical properties of the vaccine itself. Let’s have a look at some of the reasons why a vaccine can cause pain.
1. The immune response
Vaccines contain antigens from the virus, bacterium, or toxin in either a killed inactivated or a weakened live form.
- When the vaccine is injected, these antigens are introduced into the body where they are recognised as foreign, sending immune cells rushing to the injection site to build a defence in response.
- This inflammatory response, which ultimately helps to create antibodies and subsequently protects the body from the disease in the future, can cause common side effects.
- Inflammation is generated around the injection site as blood vessels dilate which can cause the redness, swelling and soreness experienced after vaccination.
- Nerves can also be irritated around the injection site causing further pain.
These side effects may not always be felt straight away but can develop over a few hours once the immune system begins to work and can sometimes last for several days. They are very common with most vaccines and demonstrate the immune system is functioning.
2. Type of Vaccine
It is thought that different vaccines can generate variable degrees of an inflammatory response, which can also possibly affect the degree of pain experienced.
- Live vaccines, which contain weakened live versions of the disease, such as the MMR vaccine, typically elicit a stronger immune response than inactivated vaccines.
- It is thought a higher immune reaction can result in increased rates of inflammation and subsequent pain experienced.
3. Route of vaccine
Another factor that can potentially influence which vaccines are more painful is the route by which they are administered.
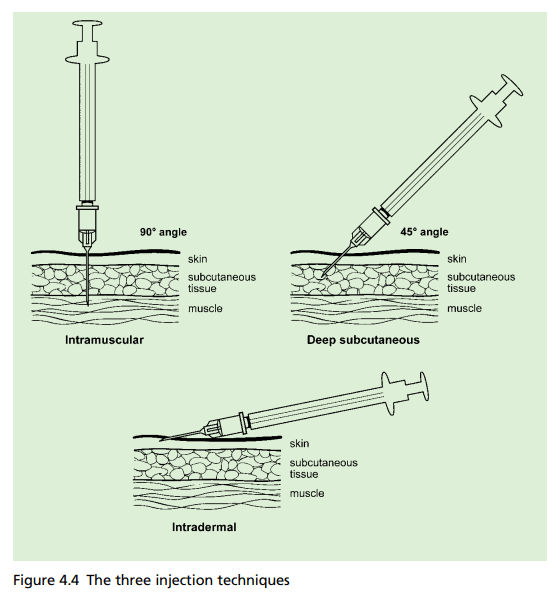
Intramuscular Injections
- With intramuscular injections, the muscle itself is made up of very tight fibres. When a vaccine is given into the muscle the needle separates these fibres, causing damage that can result in pain, swelling, and inflammation.
- Intramuscular injections also require a larger needle in order to penetrate through the several layers of skin and fatty tissue to reach the muscle, which is considered to possibly contribute towards producing more pain than other routes.
Subcutaneous Injections
- Vaccines given via the subcutaneous route are believed to be slightly less painful as they go into the layer of fatty tissue under the dermis and epidermis rather the muscle and can be reached with a shorter needle.
- Although despite this, research has shown that they may actually be more likely to induce adverse effects. According to one study looking into vaccine injection technique and reactogenicity, subcutaneous injections were often related to more injection-site responses and were more reactogenic than intramuscular injections.
- Another study comparing the immunogenicity and safety of MMR and varicella vaccines showed higher rates of injection site reactions in those that received the vaccine subcutaneously instead of intramuscularly.
- One possible reason for this is that as there are less blood vessels in the fatty tissue, the vaccine’s liquid is dispersed slower. This can also occasionally get trapped, causing possible pain.
Intradermal injection
- Intradermal injections are generally considered to be the least painful route for giving a vaccine. They use a much smaller, thinner, needle which is administered just a few millimetres under the surface of the skin into the dermis.
- Whilst they are generally associated with less pain on administration, they still can cause a stinging and painful sensation to some and redness, swelling and itching at the injection site.
4. Components of vaccine
There is some thought that it could be the components of the vaccination that may cause certain vaccinations to be more painful than others.

Adjuvants
- Adjuvants, such as aluminium salts, are used in several vaccinations to increase their effectiveness.
- Because adjuvants are formed of substances that are not naturally occurring in the body, they might trigger more immune cells towards the site of the injection, resulting in a higher immunological response.
- While this is beneficial in ensuring that the vaccination works more effectively and creates a stronger, longer lasting immunity. Some research looking into the safety of newly adjuvanted vaccines among children suggests that vaccines containing adjuvants have been shown to result in more inflammatory effects with pain being the most prevalent reported side effect.
- You can find information on the ingredients and whether adjuvants are contained in the vaccine by looking on the electronic Medicines Compendium (eMC) website. (Have a think of some of the vaccines that you may have given that are perceived as more painful and see if they contain adjuvants).
pH level
- It is also thought that the pH of the vaccination could be a contributing factor to experiencing more pain. It is considered that vaccines with a slightly acidic formulation might cause more pain at the injection site.
- This theory is also relevant when considering other injectable medications, such as certain antibiotics like penicillin which are known to be more acidic and are sometimes considered to be more painful.
5. Consistency of vaccine
Consistency is another factor that may impact how painful a vaccine feels.
- As it might be more difficult for thicker substances to get through the layers of skin and tissue, more pain is thought to be caused.
- Although not a vaccine, some may have heard of the infamous “peanut butter shot,”. A penicillin-based injection administered in the military that earnt its name because of the substance’s thick consistency and reputation for causing pain.
- It is usually recommended to administer more viscous injections more slowly to help reduce pain.
6. Volume of the vaccine
Some may believe that a higher volume of the vaccine might be a contributing factor to an increase in pain.
- A higher volume could possibly lead to more pain from the vaccine because it can put more pressure on pain receptors and can potentially cause more damage to the muscle fibres.
- It may also be perceived as more painful because it can take slightly longer to administer.
- A few studies have looked into this concept, in particular a study comparing injection pain from subcutaneous administration demonstrated an increase in pain from 1.0ml volumes in comparison to 0.5ml volume.
Other possible contributing factors that may impact pain felt from vaccines can include the speed of the injection, the needle itself and the anatomical site of the injection. It has also been thought that because vaccine’s are kept in the fridge, the colder temperature on administration can possibly cause more pain.
Which vaccines are known to be more painful than others?
This is not a well researched area, there are very few studies comparing the level of pain from certain vaccines.
- A systematic literature review looking at the pain caused by the MMR vaccines; Priorix and MMRII, concluded that Priorix caused significantly less immediate pain than MMRII (please note: MMRII is not currently used in the UK where the alternative MMRVaxPro is used instead)
- Another study looking at Order of Vaccine Injection and Infant Pain Response compared the pneumococcal vaccine (PCV), with a combined Diphtheria, Tetanus, Pertussis, Haemophilia Influenza B (DPTaP-Hib) vaccine and found that the PCV vaccine caused more pain. Interestingly it is noted in both of these studies that the more painful vaccines were slightly more acidic.
- The HPV vaccine has anecdotally been thought of as a painful vaccination and pain at the injection site is noted as a very common side effect. However a study looking at the HPV vaccine side effects and influence on completion of the three-dose regimen demonstrated similar levels of pain compared to other adolescent vaccines including tetanus and meningococcal vaccines.
With limited research available, that often leaves us as vaccinators having to rely on our individual experiences of which vaccines may cause more pain. We may do this by gathering feedback from our patients or through visual signs of pain. We may also rely on what our peers and colleagues have told us or what we may have read or heard. This highlights the need for more research to be done on this topic to enable a greater understanding of vaccine related pain and how it can be reduced.
How to reduce pain felt from a vaccine?

Does the order of injection make a difference to whether some vaccines are more painful than others?
We may feel from personal experience that certain vaccines seem to be more painful than others. There is also lots of research to show that pain can increase with repeated painful stimulation, and therefore discomfort may rise with each injection.
- Due to this, it is therefore recommended that where possible, the most painful immunisation should ideally be administered last to help reduce the overall total pain response.
- It is thought the reasoning behind this is that providing the most painful vaccination first could concentrate the attention on the process and possibly create a more intense pain signal in reaction to further vaccinations.
Whilst this is again not a heavily researched area, a study comparing DPTaP-HiB and PCV vaccine’s, showed that infants demonstrated overall less pain when receiving the PCV vaccine last.
- Although it is interesting to note that pain increased from the first to the second dose, regardless of the order of vaccines. Which backs up the theory that pain increases with each stimulus (injection) regardless.
This practice is also recommended in the World Health Organisation (WHO) Position Paper on reducing pain at the time of vaccination. However the issue is that we don’t have data for all vaccines, so how do we know which order to give them in?
WHO states that in the absence of a particular grade of the painfulness of vaccines, vaccinators should utilise their practical expertise to decide the appropriate order of injections.
What else can we do to make vaccines less painful?

1. Relax
Encourage individuals to relax their arms. It’s very normal to immediately tense up when someone is about to inject you with a vaccine. However, relaxing the muscle can ensure that it isn’t tense which is thought to contribute to pain. One good tip if someone isn’t able to relax their muscle by themselves is to gently press down on the shoulder with one hand. This encourages their arm to drop which subsequently helps the muscle to relax. For someone who is needle-phobic or prone to fainting, you can encourage them to lie down which can also help to keep the muscles relaxed.
2. Positioning
Positioning should be appropriate to the age. With infants and children, holding them in the cuddle position has been shown to reduce pain and provide comfort.
3. Skin to Skin contact/Breastfeeding in Infants
There is some evidence that skin-to-skin contact, breastfeeding and pacifiers can help reduce crying and stabilise heart rates in infants during medical procedures.
4. Distraction
There is a lot to be said of mind over matter. Helping to focus on other things and take attention away from the procedure can help to reduce pain. Children can be distracted by toys, bubbles or games on a phone. Older children, adolescents and adults can be distracted through chatting, listening to music or breathing exercises.
5. Look away!
There is some suggestion that watching the needle go in can enhance pain perception so it’s usually advised to look away!
6. Post-vaccination advice
After vaccination, encouraging movement of the arms can help to disperse the vaccine and prevent fluid from building up. However it is not recommended to massage or rub the injection site after vaccination. This is particularly important with intramuscular injections as there is a chance that it could possibly cause the vaccine to back up through the subcutaneous tissue and therefore alter its effectiveness.
Whilst pain relief isn’t recommended routinely to be given pre or post-vaccine (with the exception of MenB vaccine). If someone has soreness and pain at the injection site, then pain killers such as paracetamol or ibuprofen can be given if suitable. Ice or a cool compress can also be applied to help to reduce pain and swelling if required.
Finally, smile

If you have read all the above and are still wondering if there is anything else you can do to help relieve pain from the vaccine – maybe give this one a go! New research looking at the effects of experimentally manipulated facial expressions on needle-injection responses suggests that getting your vaccine recipients to smile can help reduce pain. (NOTE: it needs to be a big smile! – one of the ones that lift the corner of the mouth and crinkle the sides of the eyes!).
When is pain from a vaccine not normal?
Pain is a common known side effect of vaccines and demonstrates the immune system is functioning appropriately. However, whilst pain can be expected, individuals should be reminded to watch for any indications of infection or more severe adverse reactions including:
- rash appearing
- symptoms not disappearing after several days or pain becoming noticeably worse
- indications of infection such as marked redness and swelling or the injection site being hot to touch.
Although very rare, it is possible pain can be due to a shoulder injury related to vaccine administration (SIRVA), when a vaccination is given too high. This highlights the need to ensure appropriate anatomical markers are used when preparing for vaccination. Individuals with symptoms of SIRVA should be advised to seek immediate medical advice.
In summary
- Pain from vaccines can likely be contributed to many factors including the physiochemical properties of the vaccine itself, the type of vaccine, the route of administration and the overall inflammatory response.
- Research into this area in relation to specific vaccines is lacking, more studies are needed to help determine and understand more fully which vaccines are more painful and why.
- However, ultimately regardless of what the research suggests, pain is incredibly subjective and individuals perception and experiences of previous vaccination can have a huge factor in the level of pain experienced.
We know one of the barriers for some individuals in not getting vaccines is due to the perception of pain that it may cause. Whilst we may not be able to eliminate pain completely, by having an understanding of vaccine pain it can help us as vaccinators improve patient experiences and employ measures to reduce overall pain experienced.



