
Dengue (sometimes known as breakbone fever) is a viral infection caused by the dengue virus (DENV), a mosquito-borne flaviviruses which is found in tropical and sub-tropical climates, mostly in urban and semi-urban areas.
The dengue virus has four different serotypes: DENV 1, DENV 2, DENV 3, and DENV 4. Whilst human infection is often asymptomatic or causes only mild symptoms, DENV can occasionally result in more severe disease, known as dengue haemorrhagic fever (DHF), which can be fatal.
In recent years we have seen a huge upsurge of cases in a number of countries, with the disease now spreading to areas that have not traditionally reported cases. Here we will explore more about Dengue fever and look at the latest updates on the Qdenga® vaccine, which was licenced in the UK in 2023 for the prevention of Dengue fever.
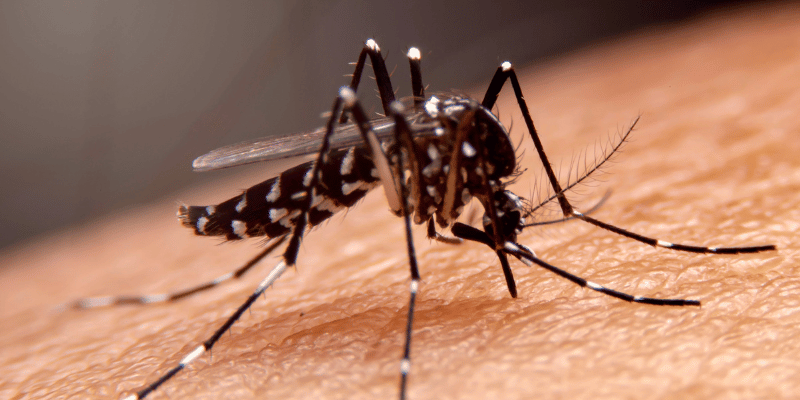
Dengue virus (DENV) is transmitted to humans primarily through the bite of infected female mosquitoes, with the primary vector being the Aedes aegypti mosquito. However, other species within the Aedes genus, such as Aedes albopictus, can also serve as vectors. In certain regions of Asia and Africa, the transmission cycle may involve jungle primates, acting as reservoirs for the virus.
Aedes aegypti and Aedes albopictus mosquitoes are closely associated with human habitats, often resting inside homes in cool, dark rooms and breeding in various water containers, including rainwater buckets, cisterns, toilets, and tires. In forested areas, these mosquitoes can be found in water-filled tree holes. While Aedes aegypti mosquitoes are typically most active during the daytime, feeding between dawn and dusk, there is a potential for them to bite at night in well-lit areas.

Symptoms of Dengue Fever typically appear 4–10 days after infection and usually last around 2–7 days. Up to 80% of those infected remain asymptomatic, while mild cases may include fever, rash, headache, muscle and joint pain, pain behind the eyes, nausea, and vomiting. A rash, often appearing on the chest, trunk, and limbs around day 3–4, is often a key diagnostic sign.
In some cases, symptoms worsen rapidly after the fever subsides, with severe dengue developing in about 5% of symptomatic cases. Severe symptoms include abdominal pain, persistent vomiting, bleeding, fatigue, rapid breathing, and cold, pale skin. It can lead to organ failure, bradycardia, and respiratory distress, especially in individuals with pre-existing conditions like diabetes, hypertension, or asthma. Severe dengue is a medical emergency requiring immediate hospital care.
Dengue treatment is primarily symptomatic and supportive. Most infections are self-limiting, with symptoms improving 3–4 days after the rash appears. Supportive treatment at home, including rest, hydration, and paracetamol for pain relief, is usually sufficient for most infections. Severe dengue requires prompt medical attention. Hospitalisation may be needed to manage fever, fluids, and blood clotting, while intensive care is essential for cases involving shock or organ failure. Early diagnosis and vigilance for severe symptoms are critical to reducing fatality risk.
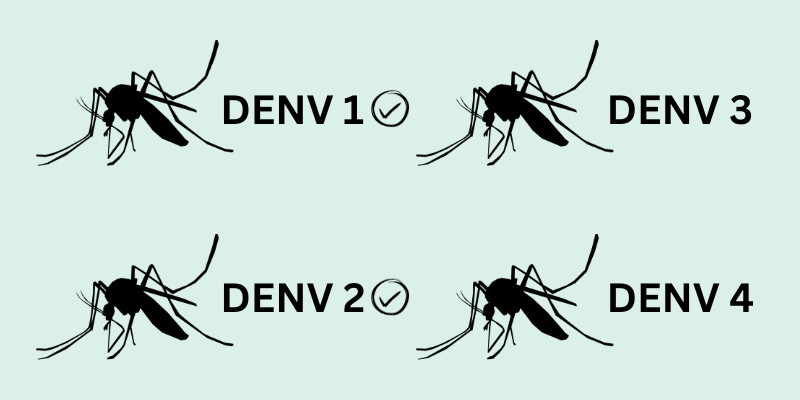
Individuals who contract the dengue virus develop a lifelong immunity to the specific serotype they were infected with. However, this immunity does not extend to the other three serotypes or to other flaviviruses. Interestingly, being infected with one DENV serotype after a previous infection with a different one can elevate the risk of severe disease through a process called antibody-dependent disease enhancement.
The global incidence of dengue has grown dramatically over the past two decades, surging more than eightfold, from 505,430 cases in 2000 to over 5.2 million in 2019. According to the World Health Organization (WHO), it is estimated that over half of the world’s population is now at risk of contracting the disease, with 100-400 million infections happening each year. The regions most severely impacted are the Americas, South East Asia, and the Western Pacific. In these areas, Dengue fever has emerged as a leading cause of hospitalisation and mortality, affecting both children and adults.

In more recent years, we have seen the disease spreading to less tropical and more temperate countries that have not traditionally reported cases. As the disease spreads to these new areas, the threat of a possible outbreak remains large.
In 2024, locally acquired cases of dengue have been documented in Italy, France, Spain and California, Florida and Texas in the USA. Large-scale outbreaks persist across countries in Central and South America. Brazil has reported the highest number of dengue cases globally, surpassing 9.8 million cases for this year as of November 2024, followed by Argentina, Mexico, Colombia and Paraguay. Dengue cases have also continued to surge in several Asian countries, including Indonesia, Philippines, Thailand and Vietnam, all seeing an increase in cases.

Several factors contribute to the increasing prevalence of dengue cases worldwide:
Rapid urbanisation, accompanied by population growth, has led to increased human-mosquito interactions in densely populated areas, contributing to the spread of the virus.
Rising temperatures and changing weather patterns create favourable breeding conditions for Aedes mosquitoes, extending their geographical range and intensifying the dengue threat. Recently unprecedented heavy rain and flooding that coincided with monsoon season has also caused a surge in cases in some countries.
Increased international travel and trade facilitate the spread of the virus across borders, makes dengue a global concern rather than a localised issue.
Travellers can spread dengue easily from one location to another and when susceptible vectors are present in these regions, local transmission can be established. This is of particular risk in that the great majority of dengue infections are asymptomatic or mild, therefore the real number of dengue cases is likely to be largely underreported or misdiagnosed for other conditions.

The main way to avoid Dengue fever is to avoid getting bitten by mosquitoes. The Aedes mosquitoes are predominantly day time biting mosquitoes, feeding between dawn and dusk. Everyone visiting areas of risk, should ensure that they take adequate insect bite avoidance precautions.


Dengvaxia®, a dengue prevention vaccine, is licensed and available in some countries for individuals aged 9–45 years but is not available in the UK. In 2017, the manufacturer, Sanofi Pasteur, reported that individuals who receive the vaccine without prior dengue infection may be at risk of severe dengue if they contract the virus after vaccination. As a result, the WHO recommends that Dengvaxia® be administered only to those with confirmed prior dengue infection.
Recently, Sanofi Pasteur announced it would discontinue production of Dengvaxia® in 2026 due to insufficient global demand.

As of January 2023, a new vaccine Qdenga®, was granted a licence for the prevention of dengue fever in individuals 4 years and over in the UK. Developed by Takeda, Qdenga® is a live attenuated vaccine that contains weakened versions of all four dengue serotypes, effectively stimulating the immune system to provide protection against dengue viruses. Notably, it has demonstrated efficacy in preventing severe dengue infection and hospitalisation.
In October 2024, the UKHSA published their guidance on the use of the Dengue vaccine in the UK in the Green Book Chapter 15a: Dengue Fever. It is currently only recommended for individuals aged 4 years and older who have had a dengue infection in the past and are either planning to travel to areas with dengue risk or ongoing outbreaks, or who are exposed to the virus through their work, such as laboratory staff handling the virus.
The JCVI has adopted a cautious approach in advising UK travellers due to the theoretical risk of severe dengue if a seronegative person is vaccinated and later exposed to the DENV3 or DENV4 strains of the virus. The primary goal is to protect individuals who are at risk of dengue and have previously been infected, from a secondary infection that could be more severe.
Detailed guidance on what qualifies as proof of a prior dengue infection and the testing requirements is available in the Green Book Chapter 15a: Dengue. This chapter also includes a helpful flowchart for investigating previous dengue infections, outlining the types of tests that can confirm infection, along with a table to assess eligibility for vaccination.
The current vaccination schedule involves administering two doses, spaced 3 months apart, which might pose a challenge for some travellers, especially those seeking last-minute travel health advice.
Qdenga® is a live vaccination and therefore specific cautions relating to live vaccines must be applied. Comprehensive information on the Qdenga® vaccine can be found in the Summary of Product Characteristics (SmPC) and the Green Book Chapter 15a.

All travellers visiting endemic countries are at risk of disease, however those who spend long periods in endemic areas (such as expatriates or aid workers) are likely at increased risk. Other risk factors may include destination, season of travel and level of exposure. Determining actual risk level is difficult and true dengue incidence in travellers is probably underestimated because in many countries dengue reporting is not obligatory and infection may go undiagnosed.

Cases in UK travellers have been on the rise. According to the UK Health Security Agency (UKHSA) research into Travel-associated infections in England, Wales and Northern Ireland: 2023, there were 634 dengue cases reported in 2023, which was an increase compared to the 448 cases reported in 2022. Most cases involved travel to Southern Asia and South-East Asia, with one case linked to travel in southern Italy.
So far this year, from January to June 2024, 473 dengue cases were reported, representing a 201% increase compared to the same period in 2023. Most cases this year have been linked to travel in Barbados, followed by Brazil, Indonesia, and Thailand.
Healthcare professionals must remain vigilant regarding dengue symptoms and consider it as a potential diagnosis in individuals who have recently returned from high-risk areas and present with symptoms such as fever or flu-like illness.

The country specific pages on Travel Health Pro (NaTHNaC) and TRAVAX should always be checked carefully for each destination and the traveller advised accordingly.
The global rise in dengue cases poses a significant challenge to public health worldwide. The introduction of vaccines like Qdenga® represents significant progress in the fight against this disease. However, its use in the general population remains limited, and further post-marketing data is eagerly awaited. To address the challenge effectively, ongoing research and improvements to existing vaccines are essential. Globally, communities continue to stay vigilant by implementing mosquito control measures and continuing to raise awareness of the disease.
We’re excited to announce the launch of our new Dengue Fever Travel Health Short Course. This course covers everything from the 5T’s of Dengue Disease to the latest recommendations for the use of the Qdenga® vaccine including practical case studies and interactive knowledge tests to deepen your understanding of testing requirements and considerations for vaccination. Here is a little taster of the course content.
Sign up today to enhance your practice and build your confidence in administering the dengue vaccine!
This Dengue vaccine training course is part of the ‘Health Academy Short Course’ series and provides clinicians with specific information related to Dengue Fever and the recommendations for use of the Dengue vaccine in the UK. This course provides 1 hour of CPD.
At Health Academy, we offer a variety of courses, both virtual and e-learning in order to help keep you up to date with the latest guidance and recommendations on Travel health. More information can be found in our Travel Health courses page.

Why not reflect on your learning from this article as part of your continuing professional development (CPD). Click below to fill out a short form which can be emailed to yourself for your own records.
Giving you written and video content to answer all your questions on primary care education from Phlebotomy to Travel Health.
Subscribe now to be kept updated with our latest posts and insights.
Start typing to search courses, articles, videos, and more.