
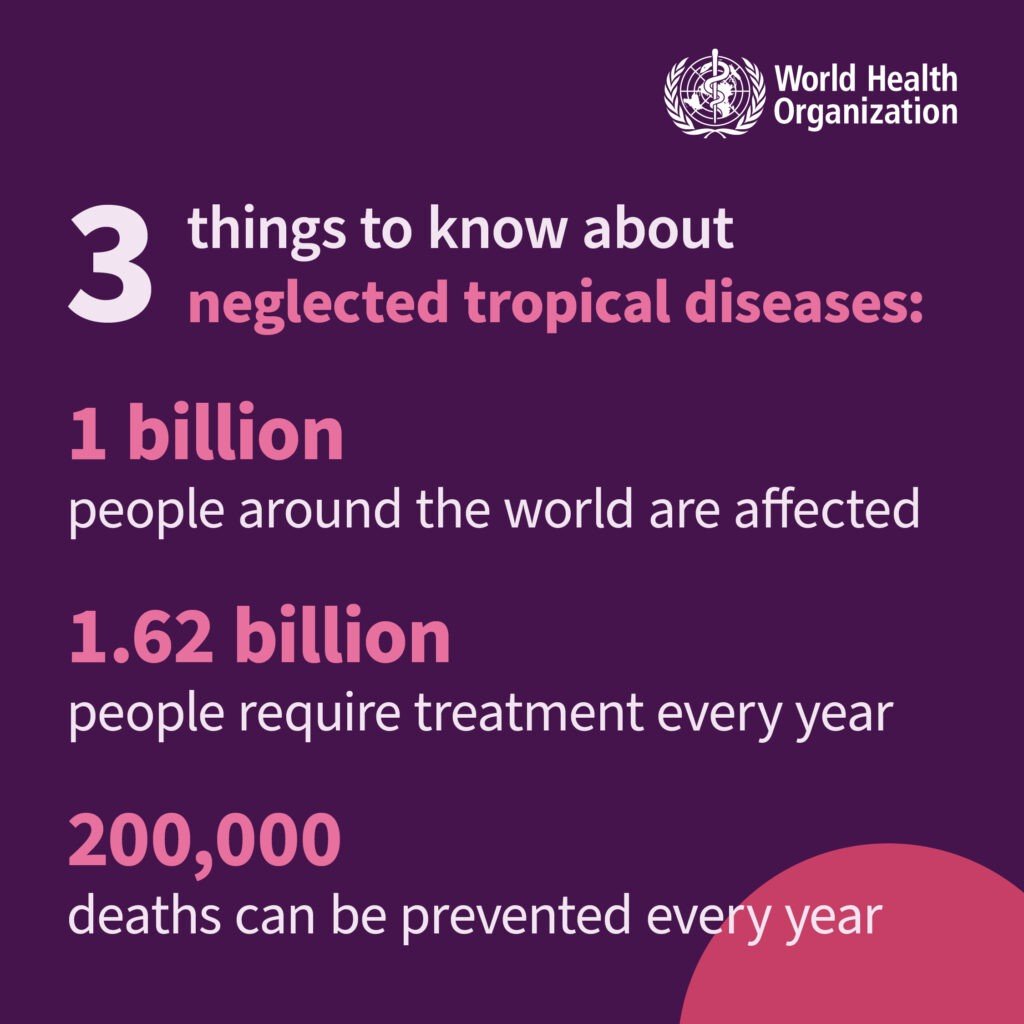
In the realms of travel health, there exists a group of diseases that are often overlooked, yet have profound implications for vulnerable populations worldwide. Neglected Tropical Diseases (NTDs) are a cluster of infectious diseases that primarily affect people living in poverty in tropical and subtropical climates. They can cause significant morbidity and mortality, impacting the lives of many and often affect marginalised communities with limited access to healthcare, clean water and sanitation. Recognising the importance of raising awareness and promoting the actions needed to eradicate the diseases, the World Health Organization (WHO) has designated the 30th January as World NTD Day.
On World NTD Day, the WHO is urging everyone, from leaders to communities, to come together and take action to tackle the disparities that fuel NTDs. The call is for bold and sustainable investments aimed at liberating approximately 1.62 billion individuals in the world’s most vulnerable communities from the relentless cycle of disease and poverty.
The WHO has put forward 21 NTD’s with the aim to alleviate the burden of these diseases on individuals and communities. Scroll through the images below to explore what these 21 diseases are.
For those of us who work in Travel Health, some of these diseases, in particular Rabies, Dengue, Chikungunya, Schistosomiasis and Leishmaniasis will be familiar to us and form part of our consultation and discussion with our travellers. But how many of the others have you heard of? let alone discuss (…or have the time to discuss) with your travellers. Yet it’s important for us to have some understanding and knowledge of NTDs and their implications, especially in the context of preventative measures for our travellers.
Buruli Ulcer: A chronic debilitating mycobacterial skin infection that can cause extensive damage to the skin, bone, and soft tissue, sometimes leading to permanent disfigurement and long-term disability. Characterised by painless open wounds, and spread by the same family of bacteria that cause Tuberculosis and Leprosy, it is common in Africa, South America and Western Pacific Regions.

Chagas Disease: A life-threatening protozoan illness transmitted to humans through various means, including contact with vector insects (triatomine bugs), ingestion of contaminated food, infected blood transfusions, congenital transmission and organ transplantation. Around 6-7 million people, mostly in Latin America are estimated to be infected with the parasite that causes Chagas disease.
Dracunculiasis (Guinea-Worm Disease): A helminth infection transmitted through drinking water contaminated with parasite-infected water fleas. The transmission cycle takes approximately a year to complete, when adult female worms painfully ulcerate through the skin, typically in the legs, to expel their larvae. Dracunculiasis was endemic in 20 countries in the mid-1980s, now it is on the verge of eradication and only found in a small number of African countries.
Echinococcosis: A parasitic disease caused by the larval stages of tapeworms forming cysts in humans. It is acquired by ingesting eggs, most commonly shed in the faeces of dogs and wild animals. Echinococcosis affects more than one million people at any given time and is found in every continent except Antarctica.
Human African Trypanosomiasis (Sleeping Sickness): A protozoan infection spread by tsetse flies, without prompt diagnosis and treatment to prevent parasites from invading the central nervous system the infection can be fatal in most. The majority of exposed people live in rural areas and rely on agriculture, fishing or hunting. It is endemic in Sub-Saharan Africa.
Lymphatic Filariasis (Elephantiasis): A helminth infection transmitted by mosquitoes, resulting in adult worms inhabiting and reproducing in the lymphatic system. It is associated with recurrent painful inflammation and abnormal enlargement of limbs and genitals. Preventive measures involve mass drug administration to at-risk populations, primarily in tropical and subtropical regions, as there is no cure once the chronic stage is reached.
Noma: A severe bacterial disease that starts as an inflammation of the gums but can rapidly progress to cause facial disfigurement. It predominantly affects children aged 2–6 years old, whilst not contagious it is often associated with malnutrition and impoverished communities. Whilst Africa bears the highest impact, instances of the disease have been documented in Asia, the Americas, and various other regions. Noma was added to the NTD list in 2023.

Onchocerciasis (River Blindness): A parasitic disease transmitted by the bite of infected blackflies, causing severe itching and eye lesions, eventually leading to visual impairment and permanent blindness. Control efforts focus on mass drug administration, aiming to interrupt transmission and alleviate the burden of this neglected tropical disease.
Trachoma: A bacterial infection transmitted through direct contact with infectious eye or nasal discharge, associated with overcrowded and impoverished communities with limited access to clean water and sanitation. If left untreated, it can cause irreversible blindness. Trachoma disproportionately affects vulnerable populations in sub-Saharan Africa, the Middle East, Asia, and parts of Latin America, emphasising the importance of public health interventions such as cleanliness, environmental improvements, and mass antibiotic distribution to curb its spread and impact.
Giving precedence to NTDs in the context of Universal Health Coverage ensures the implementation of a holistic healthcare strategy that encompasses all individuals. By strengthening health systems to combat neglected tropical diseases, they are proposing that no one is overlooked or excluded from the benefits of an inclusive and comprehensive approach to healthcare. Scroll through the below images to explore some of the intervention strategies that WHO are proposing.
As you can see from the above, the epidemiology of NTDs are intricate and frequently linked to environmental conditions and poor sanitary measures. A considerable number of these diseases are transmitted by vectors, have animal reservoirs, and are characterised by intricate life cycles. The convergence of these factors presents significant challenges in the realm of public health control.
As the world becomes more interconnected, the risk of spreading NTDs across borders also increases. Travellers may unknowingly bring these diseases from endemic regions to non-endemic areas, necessitating preventative measures and awareness. Many NTDs are transmitted by vectors such as mosquitoes and sandflies. Understanding the geographical distribution of these vectors is crucial in advising travellers on preventative measures including the use of 50% DEET and mosquito nets. Other NTD’s that are transmitted through poor sanitary conditions can be reduced by ensuring safe food and water precautions are taken. Scroll through the below images to look at ways that travellers can reduce the risk of zoonotic and vector borne NTDs.
Whilst some of these diseases may be less common to a general traveller, those travelling to remote areas, particularly healthcare workers, humanitarian workers or volunteers who may be working or living in crowded, poor and unsanitary conditions in affected countries with poor healthcare may be more at risk. Recognising symptoms of NTDs early on is essential for prompt intervention. By helping to educate our travellers on symptoms to watch for and encourage seeking medical attention promptly we can ensure they receive appropriate treatment quickly.
On WHO World NTD Day, we are are urged to recognise the significance of Neglected Tropical Diseases in the context of global health and travel medicine. A travel consultation should include a comprehensive understanding of a traveller’s destination and potential exposure to NTDs. By understanding the diverse nature of these diseases, staying informed about their prevalence in different regions, and actively engaging in discussions with our travellers, we can play a vital role in educating our travellers, breaking the cycle of neglect and improving the health outcomes of individuals globally.

If you are interested to learn more about what is going on in the world of Travel Health why not join us for a virtual Travel Health Update or sign up to one of our comprehensive online Travel Health courses – more information can be found in our Travel Health Courses page.
We have only touched very briefly on some of the 21 WHO declared NTDs. Why not try to read up on the others as part of your Continuing Professional Development (CPD). More information can be found in the WHO Neglected Tropical Diseases website. Click below to fill out a short reflective form which can be emailed to yourself for your own records.
Giving you written and video content to answer all your questions on primary care education from Phlebotomy to Travel Health.
Subscribe now to be kept updated with our latest posts and insights.
Start typing to search courses, articles, videos, and more.