Every year on the 24th March, we mark World TB Day to raise awareness about tuberculosis (TB) and the ongoing efforts to combat this preventable and treatable disease. While often overshadowed by other health concerns, TB remains a significant global health threat, claiming millions of lives annually.
This year’s theme for World TB Day; “Yes! We can end TB” underscores the importance of high-level leadership, increased investments, and the rapid adoption of new World Health Organizations (WHOs) recommendations in combating the TB epidemic and tackling health inequalities. As healthcare professionals, working across various settings from primary care to occupational and travel health we can play a crucial role in the fight against TB in every stage, from preventing the spread of the disease to diagnosing and treating those affected.

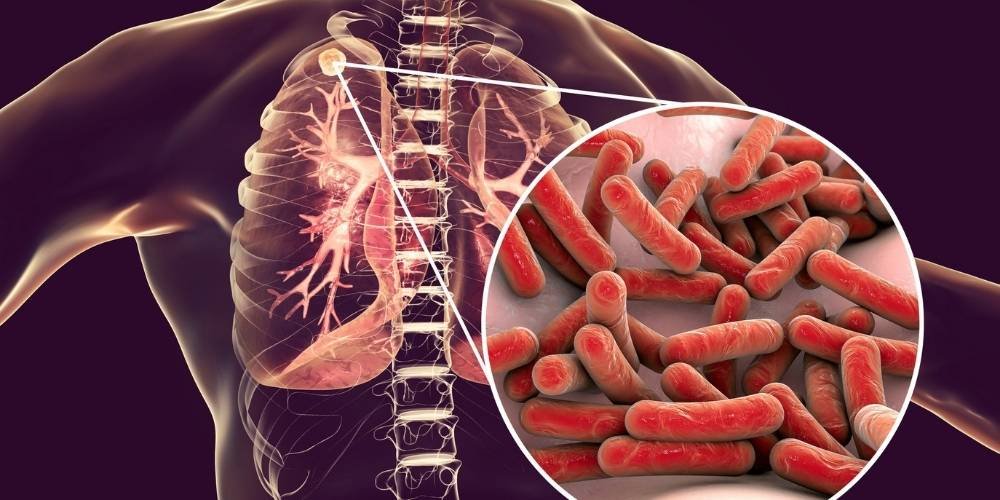
Tuberculosis (TB) is a highly contagious bacterial infection, spread by respiratory droplets caused by Mycobacterium tuberculosis. TB can either be latent or active. Active infection primarily affects the lungs but can also target other parts of the body, such as the kidneys, spine, and brain. Symptoms of active TB include a persistent cough, chest pain, fatigue, fever, and weight loss and it can be serious or potentially life-threating if untreated. However with prompt diagnosis and appropriate treatment, TB is curable, usually requiring a combination of antibiotics taken over several months. Yet, multidrug-resistant TB (MDR-TB) strains pose a challenge to treatment efforts, necessitating ongoing research and public health initiatives to control the spread of this disease.
TB remains one of the top ten causes of death in the world. More than 10 million individuals develop TB disease each year, and it is estimated that a quarter of the worlds population is currently infected with TB. TB is both preventable and curable, yet the disease is responsible for more than 1 million deaths every year, with TB being the second leading infectious killer after COVID-19 (above HIV/AIDS and Malaria) in 2022.

Source: WHO – Estimated number of deaths from infectious diseases worldwide in 2022.
The Bacillus Calmette-Guérin (BCG) vaccine is a live attenuated vaccine that is primarily used to protect against TB. The BCG vaccine has been around for many years and has been shown to be a very safe and effective vaccination. Despite TB’s significant mortality rates, the BCG vaccination continues to be the most widely administered vaccine worldwide.
TB is a global occurrence, spanning every corner of the world. In the year 2022, the majority of new TB cases were reported in the WHO’s South-East Asian Region, accounting for 46% of the total. Following closely were the African Region with 23% and the Western Pacific with 18%. Notably, more than two-thirds of the global total were reported in Bangladesh, China, Democratic Republic of the Congo, India, Indonesia, Nigeria, Pakistan, and the Philippines. TB disproportionately affects vulnerable populations, including those living with HIV, malnourished individuals, and marginalised communities with limited access to healthcare.

In the UK, from 1953, the BCG vaccination was offered to all school age children around 14 years of age and to those that were assessed as high risk. At the time of introduction about 50,000 cases of TB were reported each year in the UK, and cases occurred across the general population. The peak incidence back then was young working age adults.
Over the last 50 years the epidemiology of TB in the UK has changed from a disease that occurred across all parts of the population to one occurring predominantly in specific population subgroups, mainly those with connections to higher-prevalence areas of the world. It is estimated around 75% of UK TB patients were born abroad, with the most common countries of birth including India, Pakistan, Romania, Bangladesh and Eritrea.
Following a continued decrease in TB in the general UK population the school-based programme was discontinued in 2005. Subsequently, the programme transitioned to a risk-based approach, focusing on babies and children deemed to be at the highest risk of TB exposure. The primary objective is to prevent the occurrence of more severe forms of childhood TB through targeted immunisation efforts. Further guidance on who is recommended the BCG vaccination in the UK can be found in Tuberculosis: the green book, chapter 32.

Recent statistics published by the UK Health Security Agency (UKHSA) indicate that the incidence of TB in England stood at 7.8 per 100,000 people, falling below the WHO’s threshold for a low incidence country (less than or equal to 10 per 100,000 population). However, this wasn’t uniform across the nation, with significant concentrations observed in large urban areas, particularly in areas in London (which saw rates 17.9 per 100,000 population in 2022).
In particular, provisional data for 2023 indicates a worrying 10.7% increase in TB cases in England compared to the previous year, suggesting a rebound in TB cases exceeding pre-COVID-19 pandemic levels. This upward trend impedes progress towards meeting the WHO 2035 elimination targets.
TB continues to impact disproportionately the most economically disadvantaged communities, including groups at risk of exclusion and other health inequalities. Males, individuals with a history of imprisonment, those who experience homelessness and those with a background of substance misuse continued to have a higher likelihood of contracting TB.

Challenges in Tuberculosis control persist despite ongoing efforts to combat the disease. Among the foremost barriers are drug resistance, with strains like multidrug-resistant TB (MDR-TB) and extensively drug-resistant TB (XDR-TB) posing significant threat to TB control efforts due to the complexities of treatment leading to poorer outcomes and increased healthcare costs.
Delayed diagnosis remains a significant challenge, allowing the disease to spread unchecked within communities. Limited access to rapid and accurate diagnostic tools, coupled with the nonspecific symptoms of TB, contributes to diagnostic delays, hindering timely intervention and treatment initiation.
Moreover, stigma associated with TB can potentially deter individuals from seeking care, further exacerbating the spread of the disease. Misconceptions about TB transmission and fear of social exclusion may prevent affected individuals from accessing essential healthcare services, continuing the cycle of transmission.
Being alert to the possibility of TB is crucial. We should be especially watchful for TB in people at high risk. By promptly investigating individuals with signs and symptoms that could be TB, we can identify cases early and prevent further transmission.
Asymptomatic people who are at high risk of infection may also be screened for TB through active case-finding. Targeted screening programmes may be co-ordinated by local multidisciplinary TB teams in high prevalence settings of under-served groups, and in high-prevalence parts of the UK, such as London and the West Midlands. Latent TB screening may be recommended for certain high risk groups in the UK including close contacts of patients with TB, healthcare workers, immunocompromised patients and migrants from countries where TB is common.
Ensuring everyone has access to TB care is essential for reducing deaths caused by the disease. We should work to remove obstacles that prevent people from seeking treatment, such as distance, cost, or social stigma. This will ensure timely and appropriate care for all.
Educating patients and communities about how TB spreads, how to prevent it, and what treatment entails is crucial. By dispelling myths and reducing fear, we can encourage people to seek help early if they suspect they have TB or for those who are high risk to attend for screening and/or vaccination.
Supporting patients throughout their treatment is essential to ensure they recover fully and prevent the TB from returning. We should provide comprehensive counselling, address concerns about treatment, and monitor closely to ensure patients are taking their medications as prescribed. This helps minimise the risk of drug resistance and treatment failure, leading to better outcomes for patients.

For those of us who work in travel clinic settings, TB can often be a disease which is overlooked when discussing risks with our travellers. This is partly because of the restricted application of the BCG vaccination for travel and the limitations of other preventive measures. Nonetheless, it remains crucial to address these risks with travellers to ensure they understand how TB spreads and recognise its symptoms. This awareness enables them to be vigilant, seek medical assistance promptly, and take any necessary precautions.

Travellers can minimise their risk of TB infection by:
The risk of TB exposure for travellers depends on several things:
Country-specific information on the risk of TB can be found in the NaTHNaC Travel Health Pro Country Information pages and data from the UK Health Security (UKHSA) on Tuberculosis by country: rates per 100,000 people can help to give an idea of incidence rates by country.
On World TB Day, let us recommit ourselves to the fight against tuberculosis. Regardless if we work in primary care or a private clinic, we can help to address the challenges posed by TB and contribute in the work towards its elimination. By advocating for equitable access to care, promoting early detection and treatment, advocating and promoting vaccination for those in eligible risk groups and combating stigma, we can make significant strides in reducing the burden of TB and achieving a TB-free world.
Why not sign up for our Tuberculosis for Travel and Occupational Health course where you will learn about the 5T’s of Tuberculosis, Occupational risks, TB screening processes including BCG scar checks, Mantoux and IGRA testing and the BCG vaccination.

Giving you written and video content to answer all your questions on primary care education from Phlebotomy to Travel Health.
Subscribe now to be kept updated with our latest posts and insights.
Start typing to search courses, articles, videos, and more.