Female Genital Mutilation (FGM) is a deeply ingrained harmful cultural practice that is still carried out in certain communities across the world, mainly in some countries in Africa, the Middle East and certain parts of Asia. FGM can have serious physical, emotional and psychological implications and is illegal in the UK. As healthcare professionals, particularly those working in travel health services, we have the potential to identify young children travelling overseas who may be at danger from FGM. We also have a professional responsibility and a duty of care to protect young girls from this risk.
As we approach the summer months and the possibility of encountering those travelling for FGM increases, it is important to be reminded of the risk and what to do if FGM is suspected.
What is FGM?
FGM is defined by the World Health Organisation as:
“all procedures involving partial or total removal of the external female genitalia or other injury to the female genital organs for non-medical reasons.”
World Health Organisation (WHO, 2018)
What are the different types of FGM?
According to WHO there are four types of FGM that are practiced:
Type 1 – Clitoridectomy
This involves partial or complete removal of the clitoris and/or the prepuce.
Type 2 – Excision
This involves partial or complete removal of the clitoris and the inner labia. This can either be with or without excision of the outer labia.
Type 3 – Infibulation
This is where the vaginal opening is narrowed by creating a seal by cutting and repositioning the inner or outer labia. This may either be with or without the removal of the clitoris.
Type 4 – Other
This can include any other harmful procedures for non medical purposes. For example, piercing, incising or cauterising the genital area amongst others.
When is FGM practiced?
FGM is usually performed on young girls from infancy up to adolescence before they reach puberty. It can also be performed on young adults too, although this is not as common.
Why is FGM performed?
FGM is practised in families and communities for a variety of cultural, religious, and societal reasons. Some consider FGM to be a necessary practice for a girl to be accepted into her culture and become suitable for marriage. Some also have a mistaken belief that FGM can enhance hygiene, or they believe that the practice has religious support. Social pressure to conform to what others are doing, as well as what family members believe is necessary, can also exist.
What are the complications from FGM?
FGM is a very painful procedure that can have serious complications for the young girl which can persist into adulthood. Risk can increase with more severe forms of FGM.
Complications from the procedure itself can include:
- persistent pain
- infections
- fever
- bleeding, cysts and abscesses
- broken limbs from being held
- increased risk of HIV and AIDS
- blood loss
- shock
- death
Problems that can persist into adulthood can include:
- painful urination, repeated urinary tract infections
- discharge, itching, bacterial vaginosis and other vaginal infections
- painful menstruation or difficulty in passing menstrual blood
- scar tissue
- pain during sex and a reduced sexual desire
- difficulty conceiving and infertility
- complications during labour and childbirth
FGM can also be an extremely traumatic experience that can cause psychological effects throughout life which may include:
- depression
- anxiety
- post traumatic stress disorder
- low self esteem
- self harm
- psychosexual problems
- flashbacks to the procedure
- difficulty sleeping and/or nightmares
How common is FGM?
Although exact figures are impossible to determine, it is believed that more than 200 million girls and women alive today have had FGM. Every year, it is estimated that more than 3 million girls and young women are at risk of FGM globally. According to Forward UK, in the UK there is thought to be approximately 137,000 women and girls living with the effects of FGM and around 60,000 girls under 15 who are at risk.
In which countries is FGM performed?
The practice of FGM is known to be commonly practiced across 30 countries in Africa, the Middle East and Asia. The highest risk countries for prevalence rates includes Somalia and Guinea. In these countries a staggering 98% and 97% of young girls and women respectively have undergone FGM.
According to gov.uk, communities that are at particular risk in the UK mainly originate from:
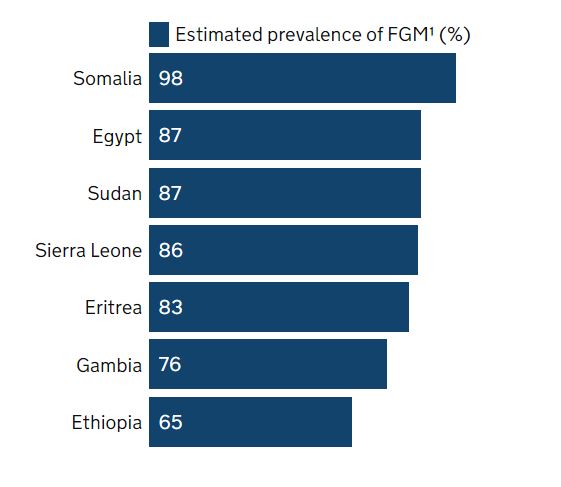
The National FGM centre have developed a helpful interactive map containing information about the prevalence rates. It also includes data on the most common type of FGM, average age performed and practising ethnic groups across the various countries. The RCN guidance on Female Genital Mutilation for Travel Health Services (Appendix 2) also contains a useful map of countries most likely to practice FGM.
Who is at risk of FGM?
Those who are at the highest risk of having FGM include those who have a family member who has had FGM already, those who are travelling to countries with high FGM prevalence or whose families originate from an FGM practising community.
It is also thought that families who are not well integrated into their community or engaged with education, healthcare and other services may be more vulnerable.
Girls are more likely to travel abroad to undergo FGM during the summer months as they will have more time to recover before returning to school. It may therefore be easier for others to misinterpret the true purposes of the trip or hide any side effects from the procedure.
Risk factors to consider include:
- Those who are travelling for long periods during the school holidays
- Those who mention that they are going on a special trip, or refer to a special procedure
- Young girls are not aware of the reason for travel or who have been asked to keep their trip a secret.
FGM and the law
FGM is illegal in the UK. It is also illegal to take a child abroad for the practice of FGM. You can also face criminal charges if you fail to prevent FGM on a girl for whom you are responsible.
- Anyone who performs FGM will face up to 14 years in prison
- The penalty for failing to prevent FGM on a girl is up to 7 years in prison
The UK government has proposed a statement opposing FGM which outlines the legal position here in the UK. This can be accessed and downloaded in a variety of languages. These can service as a useful tool to highlight the legal position of FGM and travellers can print this to take with them.
What are our responsibilities as healthcare professionals in relation to FGM?
As healthcare professionals we have a duty of care to safeguard young girls from the harm caused by FGM. All healthcare practitioners should be familiar with resources on FGM, local safeguarding policies and how to raise and action any suspected or known FGM.
Healthcare professionals, particularly those working in travel health services have the opportunity to identify young children travelling abroad who may be at risk of FGM during the pre-travel risk assessment.
FGM can be a difficult topic to approach but we should know how to discuss this with our patients in an appropriate and sensitive manner and should not be afraid to ask the right questions.
RCN Guidance on Female Genital Mutilation for Travel Health Services recommends that all travel health providers should ensure that a question on FGM is included as part of the routine pre-travel risk assessment questionnaire.
The RCN recommends using sensitive language when approaching this subject, but asking direct questions for example:
“Do you or your family members come from a community that practices FGM?”
“I see that you come from a country or area where some communities practise female genital mutilation or FGM. Do you know what FGM is? Have you been cut or circumcised?”
It is important to be mindful of other terminology for FGM, such as “cutting” or “circumcision”, or other translations from different languages. A useful translation chart can also be found in the RCN guidance (Appendix 3) which you can refer to.
What do you do as a healthcare professional if FGM is suspected/known?
All organisations should have a local safeguarding policy. The RCN FGM Travel health care pathway (Appendix 1) provides further details and a flowchart for what to do if concerns are raised during the risk assessment. It’s helpful to have this printed and easily accessible.
If you suspect that a child is at imminent risk of FGM then an urgent safeguarding response should be undertaken. In circumstances where a girl under the age of 18 discloses that they have undergone FGM, this must be reported to the police.
Healthcare workers have a legal obligation to report if FGM is discovered or if a child is believed to be a risk. Failure to report this risks being subject to “Fitness to Practice” proceedings through the organisation that regulations your profession.
In summary
FGM is illegal in the UK and is a violation of human rights and child abuse. It has no health benefits and can cause serious harm to young girls which can persist into adulthood causing long term physical, emotional and psychological effects.
Travel health consultations provide an opportunity to identify young children travelling abroad who may be at risk. As healthcare professionals working in this field, we have a professional responsibility to be aware of FGM practices and to ensure we safeguard young girls from harm. We should feel confident to be able to approach the subject of FGM, ask the right questions in a sensitive way and act on any concerns.
For more information visit our FGM Awareness and Prevention training.




