Whilst anaphylaxis following vaccination is extremely rare, it remains a risk and is a potentially life-threatening medical emergency. Early recognition and treatment is key.
All clinical staff involved in administering vaccines should be aware of the risks and how to manage a suspected anaphylactic reaction. Healthcare professionals should ensure they have receive training on anaphylaxis in accordance with Resuscitation Council UK Guidelines.
What is anaphylaxis?
Anaphylaxis is a severe allergic reaction involving multiple systems that can very quickly progress into a life-threatening situation. It happens after an individual is exposed to an allergen trigger, which may include food, insect bites or stings, medicines, or a component of a vaccination amongst others. Severe anaphylaxis is defined by a life-threatening impairment in an individuals airway, breathing and/or circulation. It can however occur without the presence of characteristic skin signs or circulatory shock.
What causes anaphylaxis?

Anaphylaxis occurs when the immune system is exposed to an allergen, which it considers to be a harmful substance. During this immune response, Immunoglobulin E (IgE) antibodies are activated which causes the release of chemicals including histamine into the body in an attempt to combat the allergen. This very abrupt and rapid release of chemicals is triggered by the immune system going into overdrive and can result in the symptoms associated with anaphylaxis.
What are the symptoms of anaphylaxis?
According to the Resuscitation Council: Anaphylaxis is likely when all of the following 3 criteria are met:
Resuscitation Council UK
- Sudden onset and rapid progression of symptoms
- Airway and/or Breathing and/or Circulation problems
- Skin and/or mucosal changes
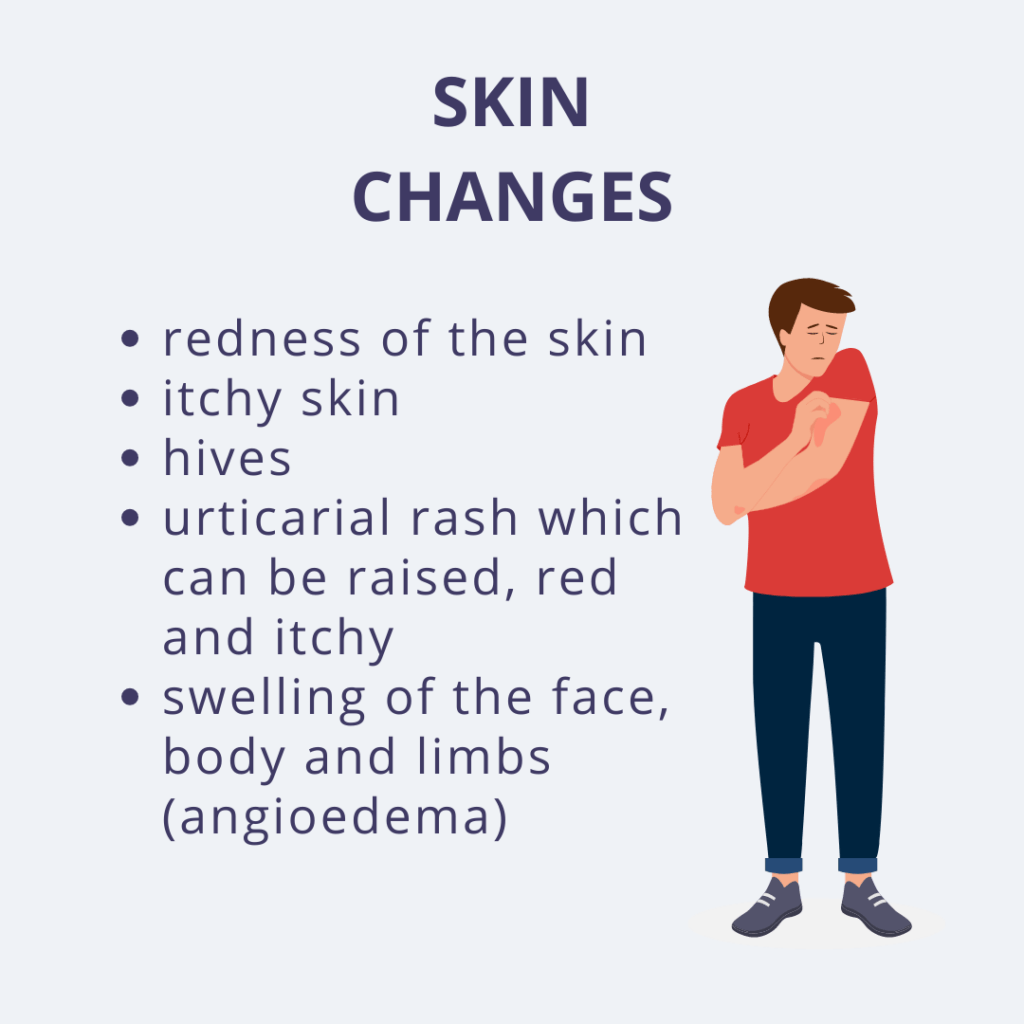
Signs and symptoms of anaphylaxis can vary. Not all symptoms are specific for an anaphylactic reaction, however it is the combination of symptoms that usually indicate an anaphylactic reaction. Possible symptoms of anaphylaxis can include:

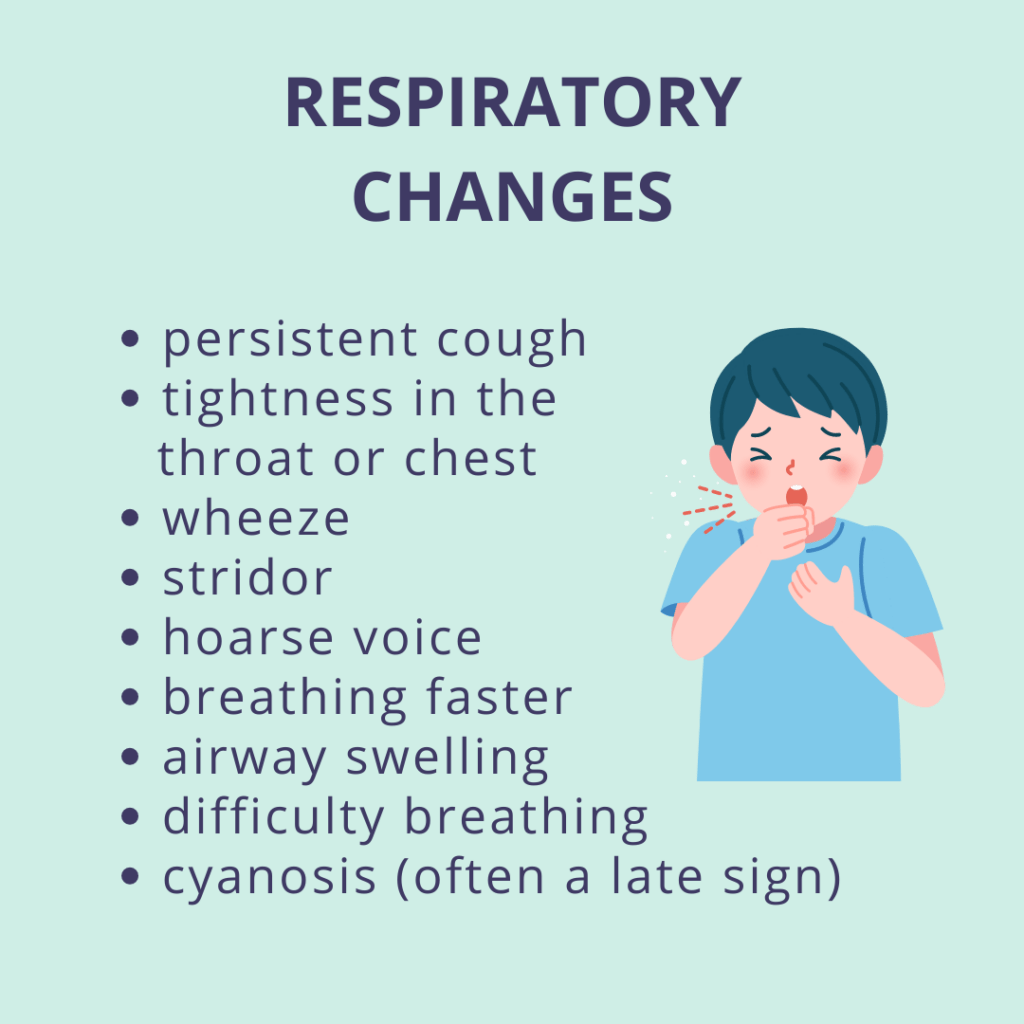
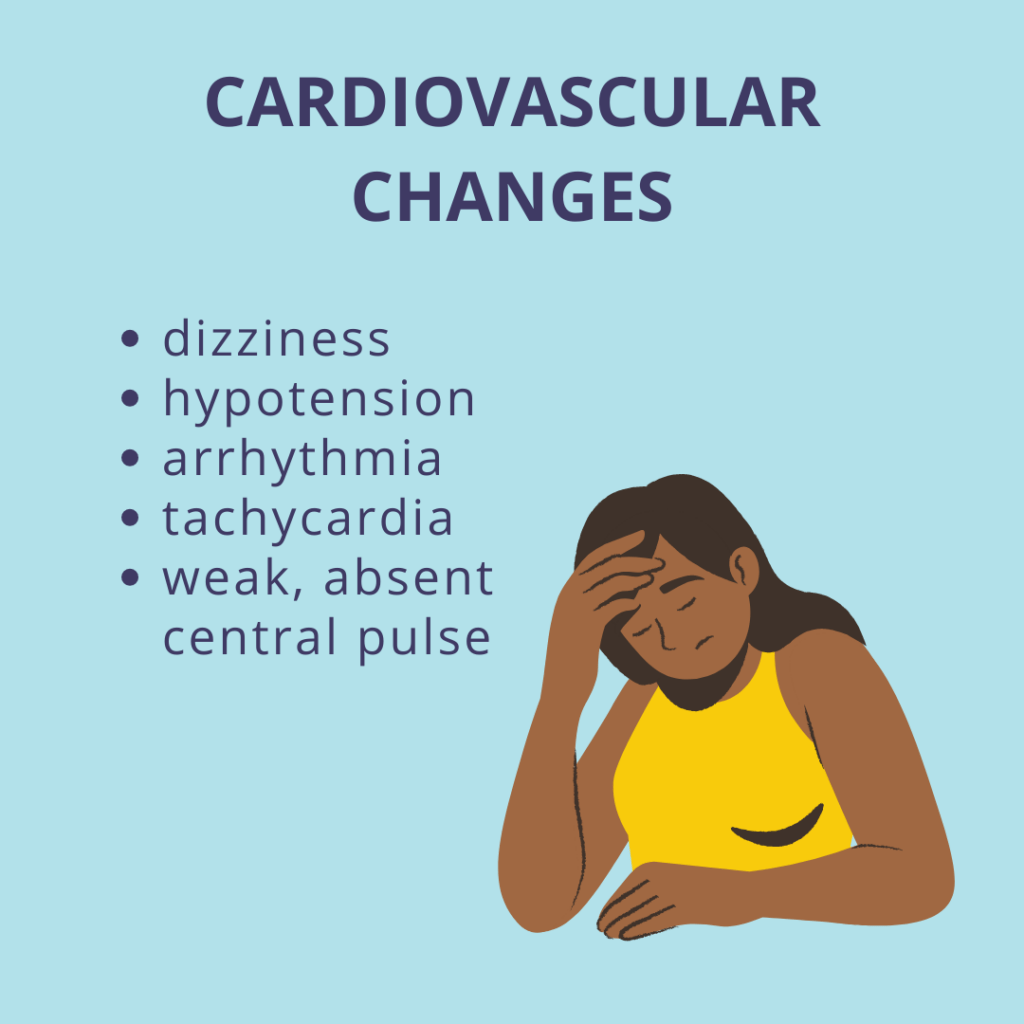
If later stages of anaphylaxis then the individual can develop hypovolaemic shock. Symptoms can include a pale and clammy appearance, low blood pressure, tachycardia and reduced peripheral perfusion. Untreated, symptoms can lead to loss of consciousness and then possible cardiac arrest.
Most presentations of anaphylaxis are multisystem with around 90% of anaphylactic reactions having skin changes. Although it is important to realise that very rarely cardiovascular collapse can happen without affecting other organs.
What are the risks of anaphylaxis following vaccination?
The incidence of anaphylaxis following immunisation is very rare. It is estimated that it may occur in fewer than 1 per million doses of vaccination given in the UK.
Are some vaccines more likely to cause anaphylaxis than others?
One study looking at whether anaphylaxis rates associated with COVID-19 vaccines are comparable to those of other vaccines found that COVID-19 vaccines ranked fifth in reported anaphylaxis rates, behind rabies, tick-borne encephalitis, combined measles-mumps-rubella-varicella (not available in the UK) and human papillomavirus vaccines. An interesting table comparing this can be found in Fig 1 of the study.
What causes anaphylaxis following vaccination?

Anaphylaxis following vaccination is thought to be most likely caused by a reaction to the vaccine components rather than the antigen itself, although this can also be a potential cause. Gelatine, yeast, egg protein, milk protein, antibiotics, adjuvants, and preservatives are common vaccination components that may trigger an allergic response in some individuals.
Some vaccinations also contain natural latex rubber in either the syringe plunger, prefilled syringe top or the vial stoppers. Contamination from latex products could be a potential cause of anaphylaxis in those who have a severe allergy. With Covid-19 mRNA vaccines, it is suspected that allergy to polyethylene glycol (PEG) and polysorbate 80 are possible risk factors for anaphylaxis.
How soon after vaccination can anaphylaxis occur?
Anaphylactic symptoms can begin within minutes of exposure to the allergen. Generally most occur within 15 minutes but less commonly they can occur within several hours.
What increases risk of anaphylaxis following vaccination?
Whilst the Green Book states that most anaphylactic reactions are thought to occur in individuals who have no known risk factors. One research study looking into the risk of anaphylaxis after vaccination in children and adults discovered that 85% of cases studied had a pre-existing atopic condition. Out of 28 recorded cases: 3 of these had previously had anaphylaxis, 16 had asthma and 9 had specified past allergies. This is also consistent with other studies that have demonstrated that co-existing atopic illness, specifically asthma, can be a clinical risk factor for anaphylaxis.
What is the treatment of anaphylaxis following vaccination?
Anaphylaxis is treated according to basic life support principles:
ABCDE (Airway, Breathing, Circulation, Disability, Exposure (ABCDE) approach must be followed and life-threatening problems treated as they are recognised.
(Resuscitation Council UK, 2008)
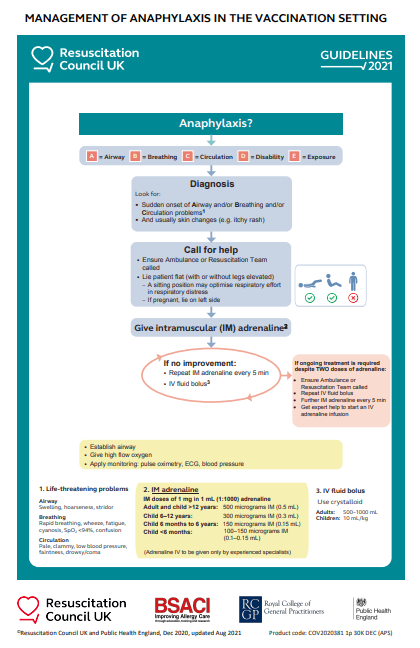
Adrenaline (epinephrine) is the main treatment in the management of anaphylaxis. It has been shown that prompt treatment is associated with increased survival.
An algorithm for the management of anaphylaxis in vaccination settings and further details can be downloaded from the Resuscitation council website.
All clinicians should be familiar with this and a copy should be made available in the vaccination clinic.
How do you know if it is an anaphylaxis or fainting (syncope)?
Fainting (syncope) can be relatively common after vaccinations in adults and teenagers. It can often happen quite quickly, usually immediately or within a few minutes of vaccination. Symptoms can include feeling lightheaded, dizzy, brief loss of consciousness and a pale appearance amongst others. Symptoms should usually resolve or improve quickly with lying down. If rapid recovery does not happen, then anaphylaxis should be suspected.
- Fainting however, is very rare in younger children and infants. Therefore, it should be assumed that a young child may be experiencing an anaphylactic reaction if they suddenly lose consciousness.
- Some individuals receiving vaccinations may also experience panic attacks. This can cause symptoms such as hyperventilation and sometimes a rash can develop which can be linked to anxiety.
It is important for clinicians to be able to distinguish between panic attacks, fainting episodes and an anaphylactic response. However if it is ever not clear, then anaphylaxis should be presumed.
Further details on the symptoms and differences between anaphylaxis and fainting can be found in our anaphylaxis course.
How to reduce the risks of anaphylaxis?

All individuals receiving vaccinations should be screened to check for any allergies. All health professionals administering vaccines should ensure that they are aware of how to access the Patient Group Direction (PGD) and the Summary of product characteristics (SPC) of the vaccine they are administering. This should be checked thoroughly to ensure there are no contraindications or precautions. Excipients and ingredients should be reviewed carefully to ensure that they are safe to administer.
What else do I need to know?
All vaccination settings should keep their anaphylaxis kit visible and within easy reach and not locked away in a cupboard. It should be checked regularly to ensure that it is within the expiry date and all staff should be familiar with the kit and it’s contents.
Alongside completing training on anaphylaxis and ensuring you are up to date with Basic Life Support, both of which are mandatory requirements when administering vaccines. You may find it helpful to participate in scenario based training in your workplace. This can include running through a practical scenario with the team where everyone acts out what they would do in the event of a patient with suspected anaphylaxis. You can take turns and switch roles and discuss different scenarios to ensure that everyone is aware of their responsibilities. This training should ideally include not just clinical staff but support staff too.
In summary
Anaphylaxis after vaccination is extremely rare and thankfully the majority of us that administer vaccines will likely never experience a case. However due to it’s life-threatening nature it is vital that all clinical staff involved in vaccinations are aware of how to manage suspected anaphylaxis and ensure that they have received appropriate training in line with Resuscitation Council UK Guidelines and have updates on this annually. You can visit our anaphylaxis course to find out more information on the training we offer at Health Academy.




