Wanting to make a move to becoming a Clinical Pharmacist in a GP surgery or a Primary Care Network (PCN) but not sure if this is really for you? These roles are becoming increasingly popular as they offer pharmacists the opportunity to grow and expand their clinical knowledge in many areas. But what does a Clinical Pharmacist ACTUALLY do?
A few years ago – I found myself dissatisfied with my role and was longing for more clinical input – I wanted to put into practice the knowledge I had gained during my degree – searching…I came across…PCN Clinical Pharmacist, GP based Clinical Pharmacist – new roles but what were they? What does a Clinical Pharmacist really do? I found the title misleading – because aren’t we all ‘clinical’? This is where my search began …. this blog will help you uncover what a Primary Care Clinical Pharmacist really does as I have discovered throughout my journey. Over 3 years in, having been both a fully patient facing PCN Clinical Pharmacist, and now a remote Senior Clinical Pharmacist… this is what my day looks like.
I start my day bright and early at 8am with my appointment ledger which has a variety of appointment types some of which require a patient call whilst others are tasks to action:

This varies in duration from 15min medication reviews and medication queries to 30 min Structured Medication Reviews (SMRs) which are more in depth holistic reviews of the patients medication and clinical condition. During these medication reviews I would discuss many aspects of their treatment. What is their compliance like? Side effects? Interactions? Is the medication having the desired effect also by ensuring the relevant blood test and monitoring elements have been completed? Do they still need this medication – if not – this medication can be stopped – this is know as deprescribing and is extremely important especially with the rise of polypharmacy – a term used to describe the situation when more people are taking a number of medicines. Let’s face it – patients often want to reduce the number of medication they are taking! This allows me to explore with the patient if the medication that was originally prescribed for a certain condition or ailment in still appropriate.
The elements checked are extensive and this is just the tip of the ice-burg but effectively what is being checked is safety and effectiveness with the patient at the heart of this, always ensuring that every contact counts!
In addition, more specific clinics are often run for certain conditions – recently I had a heart failure review clinic but the options are endless e.g hypertension clinic, HRT clinic, anticoagulation etc.
Again the duration varies from 5-15mins depending on if this is a clinical letter or discharge summary that is being actioned. This involves ensuring the medication that has been stopped/started in the latest hospital discharge is actioned. In addition, patients are often referred to different secondary care departments such as Cardiology etc and have had certain medication recommended to be initiated by the GP surgery and that’s what I then complete.

If you have worked in community pharmacy you would know the issues surrounding this! I will receive tasks throughout the day to find alternative medication to what was prescribed if currently unavailable due to shortages. Having a good relationship and open communication between myself and my Community Pharmacy colleagues is key!
When patients request a medication that is not on their repeat this would be sent to me to explore further and issue if appropriate. This often requires a conversation with the patient to assess if it is still appropriate or if there other options or factors that should be considered. Of course – if anything is outside my area of competence I am able to refer to the Duty Doctor on the day at the surgery.
Periodically I will be involved in medicines optimisation audits to ensure patient care is at its best. That might be audits on blood monitoring for certain high risk medication and whether this is being conducted in the frequency required for safe prescribing. Other audits could involve assessing if certain drugs being prescribed should be avoided because they interact with others. There is endless types of audits to be conducted. The latest I completed was assessing all patients being prescribed colecalciferol, to check if this is still appropriate whilst taking into consideration aspects such as indication, renal function, duration of treatment etc. The learning outcomes from these audits become invaluable information to ensure a better understanding of pitfalls when prescribing.
In between these clinical tasks there maybe team meetings to attend or clinical teaching sessions that involve the whole team. This gives me an opportunity to get involved in my other passion – teaching and supporting colleagues! Upskilling for a Clinical Pharmacist like any other healthcare professional is key! As an independent prescriber I am able to prescribe in my area of competence – anticoagulation in atrial fibrillation but by expanding my scope and upskilling, I am able to tackle other conditions with confidence.
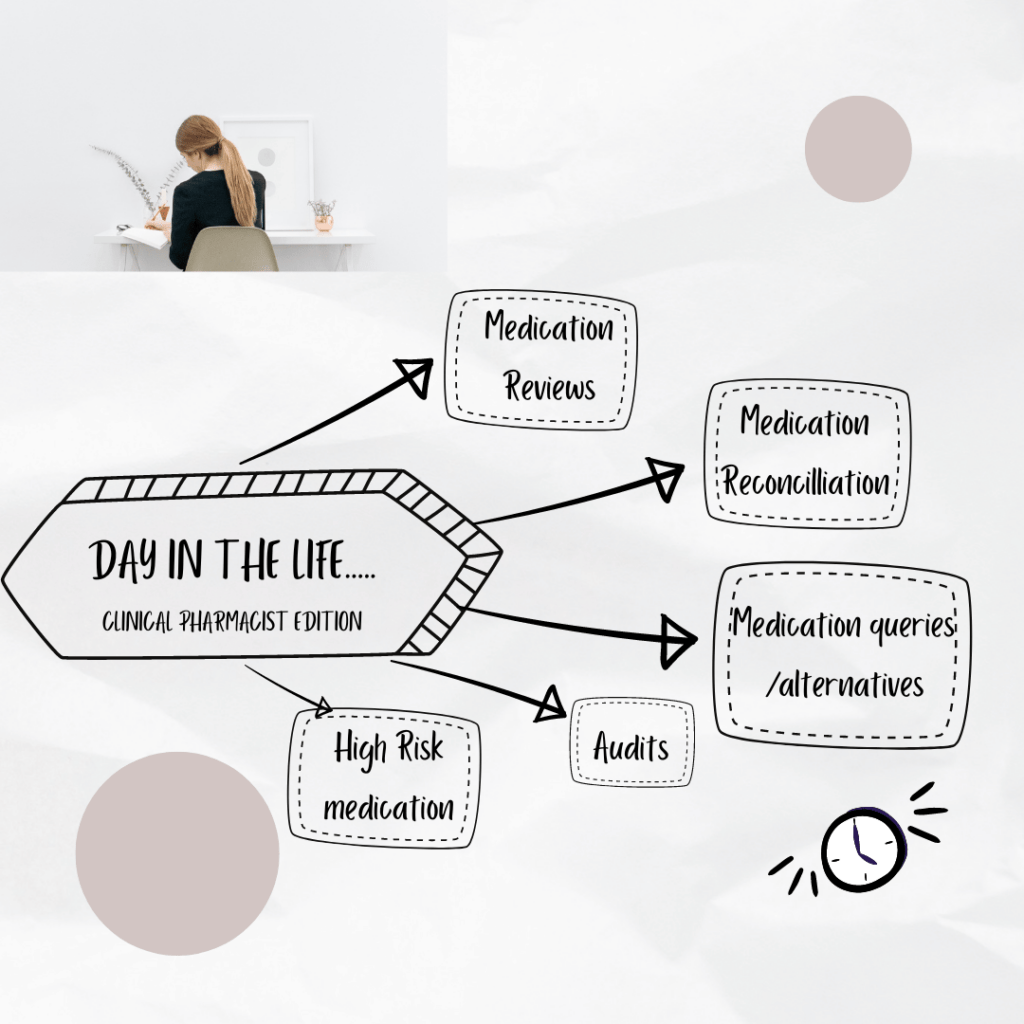
So in a nut shell …a day in the life of a Primary Care Clinical Pharmacist is very varied, with medication reviews, medicines reconciliation, acute prescription requests, communicating blood test results and much much more. Every day is different with the range of medical conditions you deal with and varying patient journeys. It is a unique opportunity to help support patients to take ownership of their medication ensuring it is optimised. The ultimate aim is improving patient care and alleviating pressures from GPs.
After all, as medicines experts this is an area we can really support in. Every day is a unique learning experience where I am upskilling myself in different clinical areas. Although my knowledge base has evolved over the years – a day in my life as a Clinical Pharmacist has been similar, but the complexity of the cases that I can take on has evolved… and this is what I love about my role! Whether you are a non-prescriber or have the independent prescribing qualification you are able to make a difference to each patients journey whilst continuing to grow in your professional career.
If this role sounds like a journey that you would like to embark on read our blog on Top 10 tips to becoming a Clinical Pharmacist!
Giving you written and video content to answer all your questions on primary care education from Phlebotomy to Travel Health.
Subscribe now to be kept updated with our latest posts and insights.
Start typing to search courses, articles, videos, and more.